Added Dietary Salt Adversely Influences Immunity & Inflammation

The Paleo community clearly is not in complete agreement on all dietary issues. One of the touchier topics is added dietary salt. A number of popular (non-scientific/non-peer review) bloggers advocate the use of refined salt or various forms of sea salt added to recipes and meals.1
Highly salted meats such as bacon are wildly popular in the Paleosphere.2 Other concentrated, salty foods such as cheese, olives, canned sardines, tuna, anchovies, caviar, salted nuts, manufactured jerky, canned tomato paste, and other salted, processed foods frequently find their way into so-called Paleo diets. You will be hard pressed to find a Paleo diet cookbook anywhere that is completely free of added, salt—that is, except for The Real Paleo Diet Cookbook (Houghton, Mifflin, Harcourt, New York, 2015).
I have written extensively on the health problems associated with added dietary salt—be it refined salt or sea salt. In the past two years startling, animal and human studies demonstrate that salt added to our diets doesn’t merely increase the risk for stroke, hypertension and heart disease,3,4,5,6 but it also adversely affects immune function, promotes chronic inflammation and represents a previously unrecognized dietary factor in the pathogenesis of autoimmune diseases.7,8,9,10,11,12
The Evolutionary Evidence of Sodium Consumption
The USDA daily recommended intake of sodium is 2300 mg. However, it must be remembered that dietary sodium and dietary salt are not equivalent. 1 gram (1000 mg) of salt (NaCl) = 390 mg of sodium. Hence 2300 mg of sodium would equal 5.9 grams of salt (NaCl).
In perhaps the most comprehensive study of hunter gatherers and non-westernized people worldwide, Denton demonstrated that their average dietary salt intake ranged from 0.6 grams to 2.9 grams of salt (NaCl) per day or 234 to 1131 mg of daily sodium.13 These numbers are derived from population-wide urinary sodium excretion rates and are considerably lower than the USDA recommended value of 2300 mg sodium per day, and much lower than the wildly speculative values (3000 to 7000 mg sodium per day or 7.7 to 17.9 grams of daily salt) suggested by a non-scientific/non-peer review Paleo blogger.1
Sodium Consumption from Contemporary, Non-Processed Foods
Consider Figure 1 below which demonstrates the sodium content of four contemporary Paleo foods: meat/seafoods (n=8), fruit (n=20) and vegetables (n=18). Note that meat/seafood averages 694 mg of sodium per 1000 kcal, vegetables 764 mg sodium per 1000 kcal and fruit 54 mg of sodium per 1000 kcal.
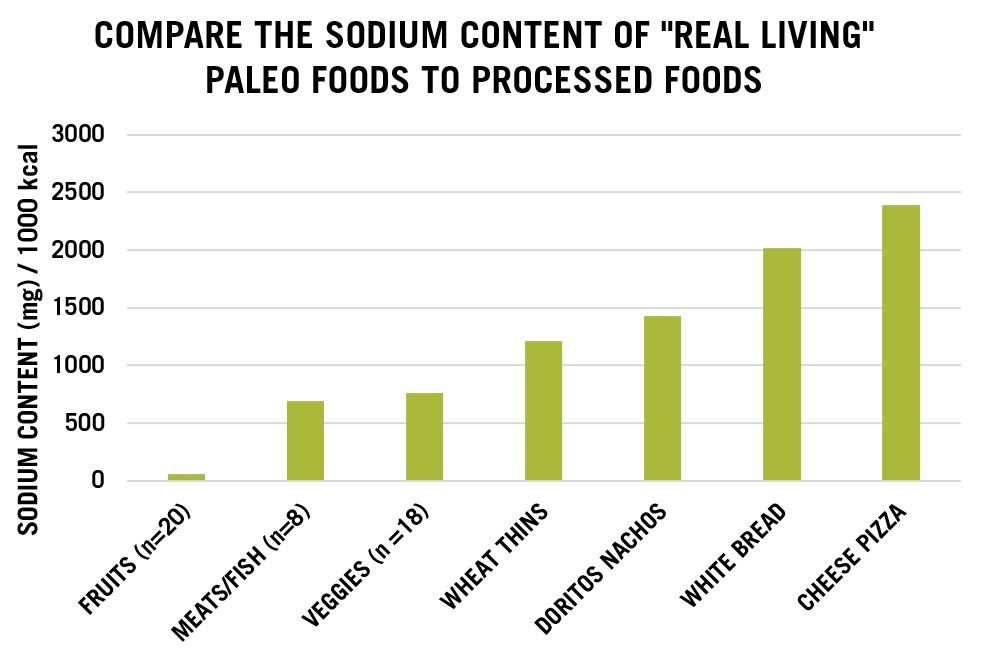
Accordingly, contemporary Paleo diets averaging 55% to 66% of daily calories (range 2200 to 3000 kcal) from animal foods and the balance from plant foods would contain sodium intakes ranging from 1600 to 2200 mg. These calculations show that unless processed foods containing added salt are consumed, it would be difficult to obtain the USDA 2300 mg recommendation for daily sodium, and almost impossible to obtain a popular bloggers’ advice (3000 to 7000 mg sodium).1
If fruits were primarily consumed in lieu of vegetables for contemporary Paleo diets, the range of daily sodium intake would be lower still (900 to 1200 mg) which falls within the values of historically studied fully, non-westernized populations.13 With contemporary Paleo foods (fresh fruits, vegetables, meats, seafood, eggs, nuts etc.) and no added salt, you will be obtaining not only sufficient sodium intakes, but also therapeutically lower sodium intakes that are consistent with values that conditioned our species’ genome over millions of years of evolutionary wisdom.
Lowered, or no consumption of added, manufactured dietary salt will lessen your risk for hypertension, stroke and cardiovascular disease,3, 4, 5, 6 certain cancers,14,15,16 and now autoimmune and immune diseases, as well as multiple diseases involving chronic low level, systemic inflammation.7, 8, 9, 10, 11, 12
Adverse Effects of Dietary Sodium upon Inflammation, Immunological Function, and Autoimmunity
I have now laid out the necessary foundation for the focus of this article. So, let’s get back into the topic at hand.
Unexpectedly, experimental studies in the past two years have provided powerful, new evidence that high salt diets cannot solely be related to hypertension, stroke , cardiovascular disease3, 4, 5, 6 and cancer,14, 15, 16 but also to diseases involving dysfunction of the immune system, chronic systemic inflammation and autoimmunity.7, 8, 9, 10, 11, 12
Let’s not forget that cardiovascular disease, cancer and autoimmune diseases cannot proceed without chronic, low level inflammation, or that the typical U.S diet is a high salt diet.17 Would it be surprising that the typical western diet which includes 70 % or more of its calories as salt laden processed foods17 and 10 to 12 grams of sodium per day5, 7, 17 might have any adverse effects upon the immune system and diseases of chronic inflammation?
The evolutionary discordance template18,19 would predict that any recently introduced dietary elements found in concentrations many standard deviations above or below those which conditioned the human genome over 2 million years of evolutionary experience, might adversely impact contemporary health and well being. Indeed is the case for immunity, inflammation and autoimmunity.
Analysis of Recent Salt Studies
In April of 2013, before my recent retirement from CSU, I awoke to a flurry of emails from scientific colleagues around the world as well as from a few of my graduate students regarding two astounding papers that had just been published in the prestigious scientific journal, Nature.8, 9 These papers represented the first experimental evidence indicating that high salt diets fundamentally altered the immune system of experimental animals in a manner that promoted autoimmune disease.
Over the past decade, numerous studies (human, animal and tissue) have implicated a specific component of the immune system (Th17 or T Helper Cell 17) in a wide variety of autoimmune diseases.20,21,22,23 The two papers on salt and autoimmunity published in Nature8, 9 were crucial, because for the first time empirical evidence demonstrated that high dietary intakes of salt were capable of up-regulating (increasing) Th17 cells in experimental animals and promoting autoimmunity.
OK—no big deal, these were just animal studies and until human studies were conducted, the link between dietary salt and the immune system, chronic low-level inflammation and autoimmunity was tenuous. The currency of science to demonstrate causality between diet and disease requires not just animal studies, but also tissue studies, epidemiological studies and most importantly experimental randomized controlled human trials.
Science typically moves slowly, but occasionally good ideas are rapidly pounced upon by scientists and researchers, thereby resulting in major leaps of knowledge. Such was the case with salt and autoimmunity.
Concurrent with the two animal studies on dietary salt and immune function8, 9 came the first human study published by Zhou and colleagues, also in April of 2013.11 Their study showed that after a 7 day (short term) high salt diet (> 15 NaCl/day) compared to a lower salt (< 5 g NaCl/day), markers (CD14++ and CD16+) of pro-inflammatory immune responses increased. CD14++ and CD16+ are molecules expressed on certain immune system cells called monocytes/macrophages.
Normally, these cells produce pro-inflammatory cytokines (hormones) when bacterial infection occurs24,25 or with autoimmune diseases.26,27 Surprisingly, even a short term (7 day) high salt diet11 caused the human immune system to become inflamed, just as if it were being attacked by foreign pathogens24, 25 or during autoimmunity.26, 27
In the most powerful human study to date, Yi and colleagues have convincingly demonstrated that a high salt diet (12 g per day) promoted a pro-inflammatory immune response whereas a lower salt intake (6 g per day) reduced these effects and caused beneficial immune system changes. The sophistication and high scientific validity of this experiment occurred because it was conducted under metabolic ward conditions over a long (205 day) duration for a simulated spaceflight program (Mars520 Mission).7
With metabolic ward conditions, each and every meal or snack are exclusively provided to test subjects. Consequently all nutrients (including sodium) are under strict control. During the experiment in an enclosed environment, daily salt intake was solely modified from 12 g/day to 9 g/day to 6 g/day for 50 + 10 days and then reversed back to 12 g/day for 30 days.
During the high salt (12 g/day) stages of the experiment, the pro-inflammatory cytokines (localized hormones) IL-6 and IL-23 increased whereas the anti-inflammatory cytokine, IL-10 decreased. Further the high salt diet caused an expansion of white blood cells (monocytes) that occur during chronic inflammation, autoimmune diseases and cancer.
On the low salt (6 g/day) diet, these deleterious immune system changes were reversed. Interestingly, during the high salt phase of this experiment, IL-17 was higher than during the low salt phase (P= 0.08). As I have mentioned earlier, numerous studies (human, animal and tissue) have implicated this specific component (Th-17) of the immune system in a wide variety of autoimmune diseases.20, 21, 22, 23
So, there you have it. The most powerful and scientifically valid study in humans has indisputably demonstrated that a high salt diet promotes chronic inflammation and adversely affects the immune system. Note that the high salt (12 g/day) phase of this experiment actually represents the normal (10-12 g/day) salt intake in the U.S.5, 7, 17 and that cardiovascular disease, cancer and autoimmune diseases cannot proceed without chronic inflammation. It is not only irresponsible for certain Paleo bloggers1 to promote high salt diets, but potentially life threatening.
References
[1] Kresser K. Shaking Up The Salt Myth: Healthy Salt Recommendations. May 4, 2012.
[2] Huntley T. The Path to Culinary Bliss: Home Cured Bacon.
[3] Strazzullo P, D’Elia L, Kandala NB, Cappuccio FP. Salt intake, stroke, and cardiovascular disease: meta-analysis of prospective studies. BMJ. 2009 Nov 24;339:b4567. doi: 10.1136/bmj.b4567.
[4] Aaron KJ, Sanders PW. Role of dietary salt and potassium intake in cardiovascular health and disease: a review of the evidence. Mayo Clin Proc. 2013 Sep;88(9):987-95.
[5] He FJ, MacGregor GA. A comprehensive review on salt and health and current experience of worldwide salt reduction programmes. J Hum Hypertens. 2009 Jun;23(6):363-84.
[6] Ando K, Kawarazaki H, Miura K, Matsuura H, Watanabe Y, Yoshita K, Kawamura M, Kusaka M, Kai H, Tsuchihashi T, Kawano Y. [Scientific statement] Report of the Salt Reduction Committee of the Japanese Society of Hypertension(1) Role of salt in hypertension and cardiovascular diseases. Hypertens Res. 2013 Dec;36(12):1009-19.
[7] Yi B, Titze J, Rykova M, Feuerecker M, Vassilieva G, Nichiporuk I, Schelling G, Morukov B, Choukèr A. Effects of dietary salt levels on monocytic cells and immune responses in healthy human subjects: a longitudinal study. Transl Res. 2015 Jul;166(1):103-10.
[8] Kleinewietfeld M, Manzel A, Titze J, Kvakan H, Yosef N, Linker RA, Muller DN, Hafler DA. Sodium chloride drives autoimmune disease by the induction of pathogenic TH17 cells. Nature. 2013 Apr 25;496(7446):518-22.
[9] Wu C, Yosef N, Thalhamer T, Zhu C, Xiao S, Kishi Y, Regev A, Kuchroo VK. Induction of pathogenic TH17 cells by inducible salt-sensing kinase SGK1. Nature. 2013 Apr 25;496(7446):513-7.
[10] O’Shea JJ, Jones RG. Autoimmunity: Rubbing salt in the wound. Nature. 2013 Apr 25;496(7446):437-9.
[11] Zhou X1, Zhang L, Ji WJ, Yuan F, Guo ZZ, Pang B, Luo T, Liu X, Zhang WC, Jiang TM, Zhang Z, Li YM. Variation in dietary salt intake induces coordinated dynamics of monocyte subsets and monocyte-platelet aggregates in humans: implications in end organ inflammation. PLoS One. 2013 Apr 4;8(4):e60332. doi: 10.1371/journal.pone.0060332. Print 2013.
[12] van der Meer JW1, Netea MG. A salty taste to autoimmunity. N Engl J Med. 2013 Jun 27;368(26):2520-1.
[13] Denton D. Salt intake and high blood pressure in man. Primitive peoples, unacculturated societies: with comparisons. In: The Hunger for Salt, An Anthropological, Physiological and Medical Analysis. Springer-Verlag, New York, 1984, pp. 556-584).
[14] D’Elia L, Rossi G, Ippolito R, Cappuccio FP, Strazzullo P. Habitual salt intake and risk of gastric cancer: a meta-analysis of prospective studies. Clin Nutr. 2012 Aug;31(4):489-98.
[15] Ge S, Feng X, Shen L, Wei Z, Zhu Q, Sun J. Association between Habitual Dietary Salt Intake and Risk of Gastric Cancer: A Systematic Review of Observational Studies. Gastroenterol Res Pract. 2012;2012:808120. doi: 10.1155/2012/808120. Epub 2012 Oct 22.
[16] Hu J, La Vecchia C, Morrison H, Negri E, Mery L; Canadian Cancer Registries Epidemiology Research Group. Salt, processed meat and the risk of cancer. Eur J Cancer Prev. 2011 Mar;20(2):132-9.
[17] Cordain L, Eaton SB, Sebastian A, Mann N, Lindeberg S, Watkins BA, O’Keefe JH, Brand-Miller J. Origins and evolution of the Western diet: health implications for the 21st century. Am J Clin Nutr. 2005 Feb;81(2):341-54.
[18] Konner M, Eaton SB. Paleolithic nutrition: twenty-five years later. Nutr Clin Pract. 2010 Dec;25(6):594-602.
[19] Frassetto L1, Morris RC Jr, Sellmeyer DE, Todd K, Sebastian A. Diet, evolution and aging–the pathophysiologic effects of the post-agricultural inversion of the potassium-to-sodium and base-to-chloride ratios in the human diet. Eur J Nutr. 2001 Oct;40(5):200-13.
[20] Burkett PR, Meyer Zu Horste G, Kuchroo VK. Pouring fuel on the fire: Th17 cells, the environment, and autoimmunity. J Clin Invest. 2015 Jun 1;125(6):2211-9.
[21] Ryu H, Chung Y. Regulation of IL-17 in atherosclerosis and related autoimmunity. Cytokine. 2015 Apr 15. pii: S1043-4666(15)00126-X. doi: 10.1016/j.cyto.2015.03.009. [Epub ahead of print]
[22] Li D, Guo B, Wu H, Tan L, Chang C, Lu Q. Interleukin-17 in systemic lupus erythematosus: A comprehensive review. Autoimmunity. 2015 Apr 20:1-9. [Epub ahead of print]
[23] Patel DD , Lee DM, Kolbinger F, Antoni C. Effect of IL-17A blockade with secukinumab in autoimmune diseases. Ann Rheum Dis. 2013 Apr;72 Suppl 2:ii116-23. doi: 10.1136/annrheumdis-2012-202371. Epub 2012 Dec 19.
[24] Rietschel ET, Schletter J, Weidemann B, El-Samalouti V, Mattern T, Zähringer U, Seydel U, Brade H, Flad HD, Kusumoto S, Gupta D, Dziarski R, Ulmer AJ. Lipopolysaccharide and peptidoglycan: CD14-dependent bacterial inducers of inflammation. Microb Drug Resist. 1998 Spring;4(1):37-44.
[25] Scherberich JE1, Nockher WA. CD14++ monocytes, CD14+/CD16+ subset and soluble CD14 as biological markers of inflammatory systemic diseases and monitoring immunosuppressive therapy. Clin Chem Lab Med. 1999 Mar;37(3):209-13.
[26] Chuluundorj D, Harding SA, Abernethy D, La Flamme AC. Expansion and preferential activation of the CD14(+)CD16(+) monocyte subset during multiple sclerosis. Immunol Cell Biol. 2014 Jul;92(6):509-17.
[27] Kawanaka N1, Yamamura M, Aita T, Morita Y, Okamoto A, Kawashima M, Iwahashi M, Ueno A, Ohmoto Y, Makino H. CD14+,CD16+ blood monocytes and joint inflammation in rheumatoid arthritis. Arthritis Rheum. 2002 Oct;46(10):2578-86.
Loren Cordain, Ph.D.
As a professor at Colorado State University, Dr. Loren Cordain developed The Paleo Diet® through decades of research and collaboration with fellow scientists around the world.
More About The Author



