Does a Low-Salt Diet Cause Insulin Resistance?

[Part Three in Our Series on the Importance of Sodium and Potassium In Our Diet]
Of all the recent developments in the Paleo nutrition world, perhaps the biggest, and most misguided, is the belief that a healthy diet includes copious quantities of salt. Some voices within the Paleosphere not only suggest that the current U.S.dietary recommendation (RDA) to consume less than 2,300 milligrams(mg) of sodium per day is wrong, but in fact, we should be eating as much as three times that recommendation.
In his blog, one popular writer stated, “I feel the data supports an intake between 3,000 and 7,000 milligrams of sodium [per day].” That“data” is a combination of theories claiming our Paleolithic ancestors consumed high quantities of salt and a few recent studies indicating that a low-salt diet may contribute to cardiovascular disease (CVD) and insulin resistance.
None of that data holds up under scientific scrutiny.
Recently, Dr. Loren Cordain performed an in-depth analysis of the sodium content of all natural foods and showed that it would have been very difficult, if not impossible, for our hunter-gatherer ancestors to have consumed even the RDA of 2,300mg/day, let alone the 7,000mg recommended by some Paleo bloggers. The ethnographic data indicates that consumption was closer to 1,000mg/day in hunter-gatherer societies. [1]
Despite the large body of research suggesting there were low salt levels in historical diets, some still look for ways to claim our Paleolithic ancestors atein excess of 3,000 mg/day. Two popular theories have developed out of a “reverse engineering” approach to the science, to back into a place where the science confirms what we want to believe. One suggests that hunter-gatherers got that sodium from animal blood. The other is that they followed wild animals to salt licks. While both sound reasonable at first, they deserve a closer look to see if they hold up under scientific weight.
An analysis of wild moose blood (a decent analogue to wild animal blood) found that 100 millilitres (ml) of blood contained 63mg of sodium. So, to get 1,000mg of sodium, you would have to drink 1.59 liters. Or, to put it in daily terms, to consume the modern RDA of sodium, you’d have to drink a gallon of blood every day. Now imagine how much blood would be required for every person in a village to get 7,000mg per day. It’s enough to make a vampire jealous.
Likewise, while the salt lick theory seems reasonable, remember that the Paleolithic era lasted over one million years. Imagine what it would take for every humanoid ancestor to get 3,000 to 7,000mg of sodium per day from salt licks for a million years. This raises the question: Just how many salt licks were there on Earth?More importantly, if they were that pervasive, why isn’t there a single mention of them in any studies of ancient villages or cultures?
Occam’s Razor states that the simplest answer is usually the correct one. And, in this case, the simple answer is clear: The large body of research shows that hunter-gatherer societies consumed around 1,000mg of sodium per day.
The New Argument: A Diet Low in Salt is Bad for Us
Other voices in the Paleosphere recommend a high-salt diet based on their claim that a low-salt diet is bad for our health. This argument was given credence by a series of studies in the early 2010s that showed a J-shaped curve relationship between salt and mortality. This J-shaped relationship indicated that people who consumed large amounts of salt had higher rates of mortality, but so did people who consumed low quantities of salt. [2-7]
We wrote a thorough analysis of these studies a few years ago, and our points are well summarized in a 2013 meta-analysis led by Graham McGregor and colleagues. The team concluded “these two papers have many methodological flaws, such as measurement error in assessing daily salt intake, confounding factors not controlled for, and reverse causality (that is, the low salt intake is the result rather than the cause of participants’ illness.)”[8]
While the J-shaped curve theory of salt consumption hasn’t been holding up in recent research, many proponents of high-salt diets are now arguing that a low-salt diet leads to insulin resistance. Several recent studies, in both rats and humans, have shown that when salt is heavily reduced in the diet, it leads to a reduction in body water which then stimulates the renin-angiotensin-aldosterone system (RAAS). That’s a mouthful, but what’s important is that an activated RAAS inhibits insulin and leads to insulin resistance. [9-14]
Interestingly, however, one of those studies, published in 2014, looked at RAAS specifically and concluded that it was “probably not a mediator of increased insulin resistance on a low-salt diet.”[9]
The Actual Data: A Low-Salt Diet May Improve Insulin Sensitivity…
Two meta-analyses written by Niels Graudaland colleagues summarized the existing research on a low-salt diet and insulin resistance and concluded there was a relationship which gave credence to the theory. [15, 16]However, McGregor and colleagues also addressed these conclusions in their 2013 paper: [8]
The meta-analysis, however, was flawed from a public health perspective, as they included a large number of short term trials with a large change in salt intake—for example, from 20g/day to less than 1g/day for only four to five days—and such metabolic studies are irrelevant to the current public health recommendations for a modest reduction in salt intake for a long period of time.
A 2016 meta-analysis published in Clinical Nutrition Research addressed the concerns of extreme sodium reduction and short study lengths.[11]The authors divided 25 studies on low-sodium diets and insulin resistance into short-term vs. long-term studies and extreme salt restriction vs.moderate reductions.
The results are shown in Table 2, copied from the meta-analysis, below:
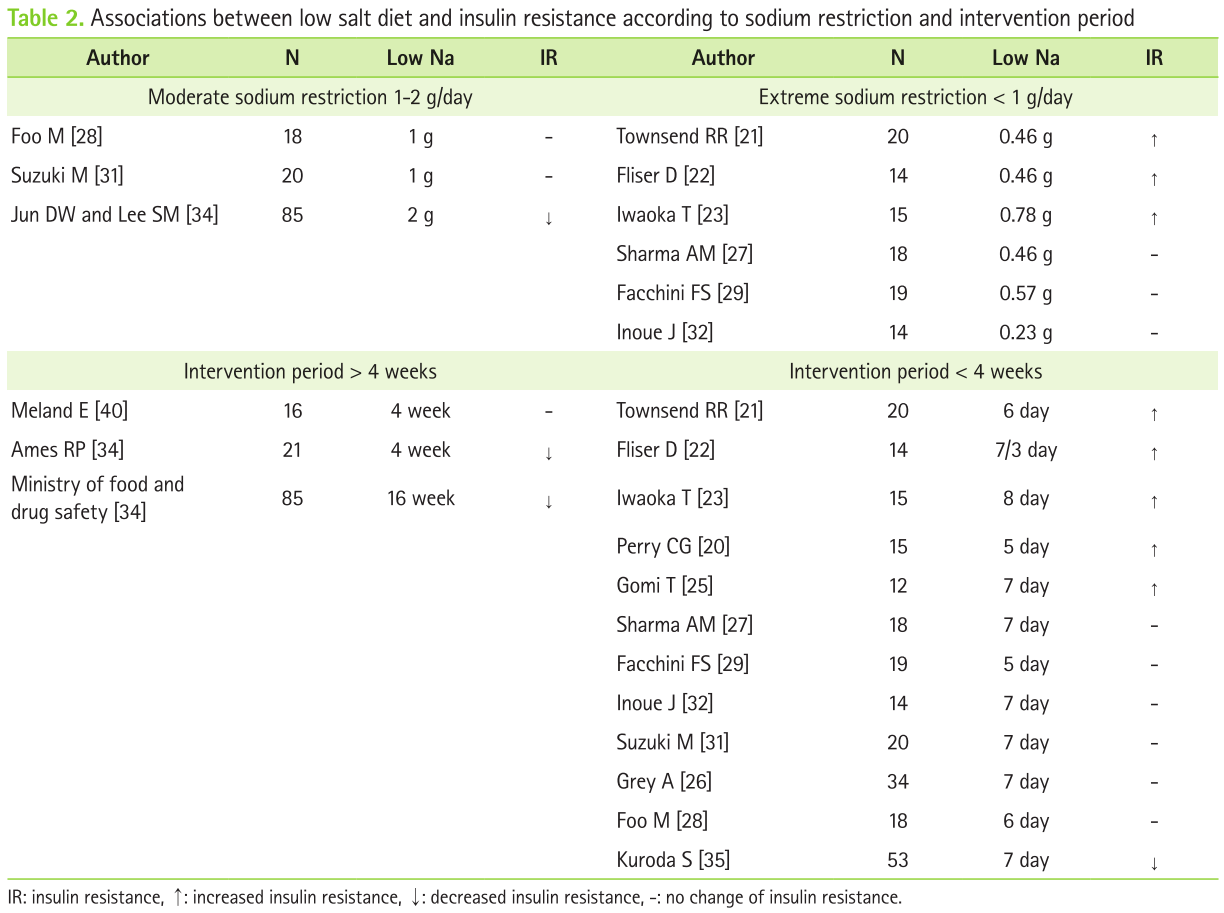
It is important to note that for the purposes of the analysis, the authors defined “moderate reduction” as 390 to 780mg of sodium per day—in line with the low end of what has been seen in hunter-gatherers’ diets. Studies with extreme salt-restriction limited consumption to less than 390mg/day—below the recommended minimum intake. Even the 2014 study looking at RAAS activation on a low-salt diet admitted in their methodology: “10 mmol/day sodium is at the extreme lower end of the physiological range of sodium intake and not practical for long term use.”
In Table 2, studies that concluded a low-salt diet contributes to insulin resistance were all in the short term column and almost all were in the extreme sodium restriction column. As the authors point out, the human body will react to any extreme change in the short run.Short-term insulin resistance might simply be a temporary result of a sympathetic stress response and not something that would continue in the long term.
To further make this point, all the studies that used moderate sodium restriction or were carried out over a long term had either no impact on insulin resistance or, in three cases, improved insulin resistance.
A High-Salt Diet May Make Insulin Sensitivity Worse
A 2018 study in the journal PNAS addressed the question of salt and insulin resistance. However, this study was exploring ways in which a high-salt—not a low-sa—diet might cause insulin sensitivity. The study stated that “in contrast to short-term studies, long-term intake of a high-salt diet is associated with increased frequencies of obesity, insulin resistance, nonalcoholic fatty liver disease, and metabolic syndrome.” [17]
Without diving deep into the mechanism, the authors of the study found that feeding mice a one percent salt solution for 30 weeks increased their natural production of fructose. Fructose is associated with insulin resistance, diabetes, and obesity.
Another 2018 study written by ZhaofeiWan et. al. looked at how a high-salt diet may contribute to insulin resistance in humans. They found that feeding subjects 18g of salt per day activated NLRP3 inflammasome, which in turn promoted a form of inflammation associated with insulin resistance. [18]
To be fair, this study was also a one-week study and the effects may also be a short-term reaction to increased salt consumption. But, even if it is just short term, another interesting discovery of the study was that taking 4.5g/day of potassium along with the added salt seemed to undue many of the inflammatory effects of the high-salt diet.
In Short:The Data Continues to Show That a Healthy Diet is Low in Salt and High in Potassium
Sodium is an essential nutrient; we need it to survive. But we must be careful not to translate that into a “more is better” approach by pointing to the health benefits of consuming adequate levels of sodium and extrapolating from there. In the case of sodium, more is not better, and a very convincing body of science shows that 7,000mg/day contributes to a slew of health problems, including insulin resistance.
The 2018 study by Wan et. al. focused, for the first eight pages, entirely on inflammatory markers, reactive oxygen species, and the effects of salt on THP-1 monocytes. In short, if you’re looking for a nerdy read from a bunch of scientists holed up in a lab, this is not one to miss.
So, it was interesting to see them take a very Paleo turn in the discussion section of their article. They state: “increasing evidence suggests that compared with prehistoric or primitive humans, modern people with more sodium and less potassium intake are more vulnerable to suffering from CVD.”
Their final recommendation stated that “potassium is abundant in fresh fruits and vegetables. Therefore, a greater fresh fruit and vegetable consumption and reasonable salt restriction could protect against the occurrence of insulin resistance and CVD.” This squarely coincides with The Paleo Diet.We hope this recommendation begins to persuade more people to reconsider their sodium intake.
Read More in Our Series on Sodium and Potassium in the Diet:
-
The Sodium/Potassium Ratio and its Importance in Human Health By Mark J. Smith, PhD
-
The effects of salt substitute on community-wide blood pressure and hypertension By Dr. Marc Bubbs ND, MSc, CISSN, CSCS
-
Recipe: Blueberry and Roasted Beet Kale Salad By Lorrie Cordain
References
- Denton, D., Salt intake and high blood pressure in man. Primitive peoples, unacculturated societies: with comparisons, in The Hunger for Salt, An Anthropological, Physiological and Medical Analysis. 1984, Springer-Verlag: New York. p. 556-584.
- O’Donnell, M., et al., Urinary sodium and potassium excretion, mortality, and cardiovascular events. N Engl J Med, 2014. 371(7): p. 612-23.
- O’Donnell, M.J., et al., Urinary sodium and potassium excretion and risk of cardiovascular events. JAMA, 2011. 306(20): p. 2229-38.
- Pfister, R., et al., Estimated urinary sodium excretion and risk of heart failure in men and women in the EPIC-Norfolk study. Eur J Heart Fail, 2014. 16(4): p. 394-402.
- He, F.J., et al., Does reducing salt intake increase cardiovascular mortality? Kidney Int, 2011. 80(7): p. 696-8.
- He, F.J. and G.A. MacGregor, Cardiovascular disease: salt and cardiovascular risk. Nat Rev Nephrol, 2012. 8(3): p. 134-6.
- Stolarz-Skrzypek, K., et al., Fatal and nonfatal outcomes, incidence of hypertension, and blood pressure changes in relation to urinary sodium excretion. JAMA, 2011. 305(17): p. 1777-85.
- He, F.J., J. Li, and G.A. Macgregor, Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ, 2013. 346: p. f1325.
- Garg, R., B. Sun, and J. Williams, Effect of low salt diet on insulin resistance in salt-sensitive versus salt-resistant hypertension. Hypertension, 2014. 64(6): p. 1384-7.
- Prada, P.O., et al., Low salt intake modulates insulin signaling, JNK activity and IRS-1ser307 phosphorylation in rat tissues. J Endocrinol, 2005. 185(3): p. 429-37.
- Oh, H., et al., Low Salt Diet and Insulin Resistance. Clin Nutr Res, 2016. 5(1): p. 1-6.
- Townsend, R.R., S. Kapoor, and C.B. McFadden, Salt intake and insulin sensitivity in healthy human volunteers. Clin Sci (Lond), 2007. 113(3): p. 141-8.
- Fliser, D., et al., The effect of dietary salt on insulin sensitivity. Eur J Clin Invest, 1995. 25(1): p. 39-43.
- Iwaoka, T., et al., The effect of low and high NaCl diets on oral glucose tolerance. Klin Wochenschr, 1988. 66(16): p. 724-8.
- Graudal, N.A., T. Hubeck-Graudal, and G. Jurgens, Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride. Cochrane Database Syst Rev, 2011(11): p. CD004022.
- Graudal, N.A., T. Hubeck-Graudal, and G. Jurgens, Effects of low-sodium diet vs. high-sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride (Cochrane Review). Am J Hypertens, 2012. 25(1): p. 1-15.
- Lanaspa, M.A., et al., High salt intake causes leptin resistance and obesity in mice by stimulating endogenous fructose production and metabolism. Proc Natl Acad Sci U S A, 2018. 115(12): p. 3138-3143.
- Wan, Z., et al., Involvement of NLRP3 inflammasome in the impacts of sodium and potassium on insulin resistance in normotensive Asians. Br J Nutr, 2018. 119(2): p. 228-237.
Trevor Connor, M.S.
Dr. Loren Cordain’s final graduate student, Trevor Connor, M.S., brings more than a decade of nutrition and physiology expertise to spearhead the new Paleo Diet team.
More About The Author