The Importance of the Magnesium and Calcium Relationship: A Key Ratio for Health
The magnesium and calcium relationship is an important underlying concept of The Paleo Diet and Dr. Loren Cordain’s thirty years of nutrition research. In fact, the calcium-to-magnesium ratio is a key reason that dairy products are not Paleo foods. Unfortunately, 1970s-era government-backed daily nutrition guidelines that were intended to address osteoporosis got the nutrition science wrong and missed a key point; the ratio of magnesium and calcium matters far more than total calcium for bone health. Most people get too much calcium and not enough magnesium. Worse yet, too much calcium (or not enough magnesium) can cause many chronic health problems including heart disease, cancer risk, insulin resistance, and inflammation.
We need calcium. No one is going to dispute that fact. Calcium is the most abundant mineral in our bodies, critical to bone health and muscle function. (1,2) Without adequate calcium we could not survive. So, it is no wonder that for several decades, the need for calcium (either through diet or supplementation) has been promoted for good health—from milk moustache advertisements touting strong bones to osteoporotic women being told to supplement by their doctors.
The result of this increased awareness is that daily calcium intake nearly doubled in women from 1977 to 2011. Much of that increase was due to supplementation. (3)
So, what impact did this awareness have on health? The increased calcium consumption, particularly from milk, has been associated with a higher risk of heart disease, cancer, insulin resistance, inflammation, and all-cause mortality. (4–11) And while many are increasing their calcium intake to strengthen their bones, evidence that higher calcium consumption prevents bone degeneration or factures is limited and sometimes contradictory. (7,12)
Does this evidence suggest that calcium is actually bad for us? Of course not. Calcium is essential for life. But as with all things in nutrition, it’s not a simple matter of “more is better.” This is best summarized by a 2018 concept paper in the highly respected journal Nutrients:
[This] goes beyond the classical approach of evaluating each micro or macro nutrient by itself; which may be a relic of the past when deficiency type studies dominated… Micronutrient ratios may confer more comprehensive information than the concentration of a single nutrient… This suggests that the underlying issue is a disruption in the ratios of micronutrients in the Western diet. (13)
Which brings us to the calcium-to-magnesium ratio. What may be more important than the absolute quantity of calcium in the diet, or magnesium for that matter, is a healthy ratio of the two.
Most People Get More Than Enough Calcium And Not Enough Magnesium
The same 2018 paper showed, using NHANES data, that men over the age of 50 consumed 1,589 mg/d of calcium compared to the recommendation of 1,000 mg/d, while women over 50 consumed 1,177 mg/d compared to the 1,200 mg/d recommended.
In short, looking purely at their calcium intake, the subjects were getting enough. Yet, in the general population, osteoporosis has been on the rise. So, there is more to this issue than the absolute quantity of calcium.
Which brings us to the magnesium and calcium relationship. What may be more important than the absolute quantity of calcium in the diet, or magnesium for that matter, is a healthy ratio of the two. In the same period from 1977 to 2011, the ratio in women increased from approximately 2.6-to-1 up to 3.7-to-1. This is illustrated in Figure 1 below:
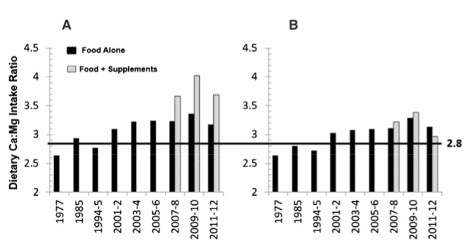
Extensive research on the subject has shown that a ratio of approximately 2-to-1 calcium-to-magnesium ratio is considered healthy, while ratios above 2.6-to-1 and below 2-to-1 can lead to heart disease and other conditions. (3,14) Several recent studies showed decreased mortality rates when magnesium intake was increased by 200 mg/d or more in subjects with a 3-to-1 or higher ratio. (15–17)
The importance of a healthy magnesium and calcium relationship may explain the contradictory results seen in research studies that only looked at calcium concentrations. High, low, and recommended calcium consumption has been inconsistently shown to contribute to heart disease. The results may have more to do with the calcium-to-magnesium ratio, as explained in the 2016 review by Rosanoff et al.:
Dietary intake studies of either magnesium or calcium alone may be unwittingly confounded by the unmeasured calcium or magnesium… it appears that too much or too little of either calcium or magnesium might not be beneficial and there may be an optimal range of human calcium and magnesium intake. (3)
In the United States, the average calcium-to-magnesium ratio is above 3-to-1 and frequently higher in women. In Japan, the ratio is below 1.7-to-1. Both levels are considered unhealthy. (3)
Why More Calcium—Without More Magnesium—Is Dangerous for Health
In an effort to stop rising osteoporosis rates in North America, as previously mentioned, calcium RDAs were increased in women to 1,200 mg/d. Other recommendations have even taken it higher to 1,300 mg/d. Calcium is the only RDA where the recommendation is higher for women than for men. See the National Institutes of Health U.S. RDA tables.
There are several problems with this strategy. First, there are risks associated with increasing calcium intake in isolation. Two recent studies in BMJ demonstrated this risk. The first, a 2010 meta-analysis of 26 studies, clearly showed that calcium supplementation increases the risk of both heart attacks and sudden death. (8)
The second, a 2013 cohort study of over 61,000 women, found that high calcium intake increased the death rates from all-cause mortality in women. (6) However, conversely, a 2011 randomized controlled trial found that calcium supplementation in women over 70 did not find an increased risk of vascular disease. (18)
The second problem with increasing calcium in isolation is that it is nearly impossible to achieve these RDAs for calcium on a natural diet without either consuming dairy or supplementing. (5)
Dr. Cordain has written extensively about milk and how it contributes to a host of health issues including heart disease, acne, cancer, and insulin resistance. (4) In short, dairy has a calcium-to-magnesium ratio of around 12-to-1, which is the highest of any food we eat. So, drinking milk regularly may help you meet the RDAs for calcium, but it is only going to push this critical ratio into more unhealthy ranges.
Dairy has a calcium-to-magnesium ratio 6x higher than our ancestral diet.
—Research by dr. loren cordain
In fact, a 1993 study by Dr. Artaud-Wild et. al, found that milk and its components (including calcium) had the highest relationship with cardiovascular death rates of any food examined. (19)
You may be following your doctor’s advice by consuming more milk and supplementing with calcium, but without proportionally increasing your magnesium consumption, the results could be devastating. And this is a concern because it appears that over 50 percent of Westerners get inadequate magnesium. (3)
The Optimal Calcium-to-Magnesium Ratio
Americans do not get sufficient magnesium. Furthermore, the typical Western diet has a calcium-to-magnesium ratio above 3-to-1. (3) The solution for most of us is to increase magnesium consumption.
That raises the question: How much more magnesium do we need? Unfortunately, that’s difficult to answer. Our bodies maintain a very tight magnesium concentration in our blood. If we do not eat enough, our bodies will sacrifice bone and intracellular stores in order to maintain plasma levels. As a result, people can be magnesium deficient while still having normal serum levels—a condition called “chronic latent magnesium deficit” or CLMD. (3)
Unfortunately, simply supplementing with magnesium is often not a solution. It’s important to get a ratio of calcium-to-magnesium around 2-to-1. Straying too high or too low from that ratio is unhealthy. But since most people don’t know how much calcium or magnesium they are getting in their diet and there isn’t a good blood test to determine our magnesium levels, it’s hard to know how much to supplement. Furthermore, according to Rosanoff et. al., adults who supplemented with magnesium overcompensated with calcium and made their calcium-to-magnesium ratio worse. (3)
Ultimately the best solution is through a natural diet. (26) Analyses of hunter-gatherer diets have shown that daily intake approximated the optimal ratio of 2-to-1. (14)
Since, for most North Americans, the issue is bringing down the ratio below 3-to-1, eating fruits, vegetables, and nuts (such as almonds), which are high in magnesium, can help you get adequate magnesium in your diet while also ensuring you obtain the calcium you need for an optimal ratio and good bone health.
Dr. Loren Cordain created the following two tables of fruits and vegetables showing their calcium-to-magnesium ratios as a guide.
Common Vegetables and Their Mg and Ca Content
TABLE 1: calcium and magnesium content and calcium-to-magnesium ratio of common vegetables sorted by ratio
| Vegetables, Domesticated |
Mg/100g | Ca/100g | Ca/Mg |
|---|---|---|---|
| Mushrooms, white | 9.0 | 3.0 | 0.33 |
| Tomatillo | 20.0 | 7.0 | 0.35 |
| Sorrel | 102.1 | 44.0 | 0.43 |
| Artichoke | 42 | 21.0 | 0.50 |
| Sweet potato leaves | 61.0 | 37.0 | 0.61 |
| Swiss Chard |
81.0 | 51.0 | 0.63 |
| Eggplant | 14 | 9.0 | 0.64 |
| Squash, Crookneck | 27 | 20.0 | 0.74 |
| Jalapeno pepper | 15 | 12.0 | 0.80 |
| Squash, Summer | 17.0 | 15.0 | 0.88 |
| Squash, zucchini | 18.0 | 16.0 | 0.89 |
| Tomato | 11.0 | 10.0 | 0.91 |
| Purslane | 68.0 | 65.0 | 0.96 |
| Bell pepper | 10 | 10.0 | 1.00 |
| Pumpkin leaves | 38 | 39.0 | 1.03 |
| Squash, Acorn | 32.0 | 33.0 | 1.03 |
|
Cucumber | 13.0 | 16.0 | 1.23 |
| Spinach | 79.0 | 99.0 | 1.25 |
| Kohlrabi | 19 | 24 | 1.26 |
| Squash, butternut | 29 | 41 | 1.41 |
| Okra | 57 | 81.0 | 1.42 |
| Radicchio leaves | 13.0 | 19.0 | 1.46 |
| Cauliflower | 15 | 22.0 | 1.47 |
| New Zealand Spinach | 39.0 | 58.0 | 1.49 |
| Beet greens | 70.0 | 117.0 | 1.67 |
| Asparagus | 14.0 | 24.0 | 1.71 |
| Pumpkin | 12 | 21.0 | 1.75 |
| Palm hearts | 10.0 | 18.0 | 1.80 |
| Brussel sprouts | 23 | 42.0 | 1.83 |
| Squash, Spaghetti | 11.0 | 21.0 | 1.91 |
| Broccoli | 21.0 | 47.0 | 2.24 |
| Romaine lettuce | 14.0 | 33.0 | 2.36 |
| Iceburg lettuce | 7 | 18.0 | 2.57 |
| Butterhead (Bibb) lettuce | 13.0 | 35.0 | 2.69 |
| Lettuce, red leaf | 12 | 33 | 2.75 |
| Parsley | 50.0 | 138.0 | 2.76 |
| Loose leaf (Green Leaf) lettuce | 13.0 | 36.0 | 2.77 |
| Cabbage, red | 16 | 45.0 | 2.81 |
| Fennel bulb | 17 | 49.0 | 2.88 |
| Mustard greens | 32.0 | 103.0 | 3.22 |
| Chicory greens | 30 | 100.0 | 3.33 |
| Cabbage, green | 12 | 40.0 | 3.33 |
| Arugula | 47 | 160.0 |
3.40 |
| Endive (Escaroie) | 15.0 | 52.0 | 3.47 |
| Celery | 11.0 | 40 | 3.64 |
| Grape leaves | 95 | 363.0 | 3.82 |
|
Kale | 34.0 | 135.0 | 3.97 |
| Rapini (Broccoli Raab) | 22.0 | 108.0 | 4.91 |
| Dandelion greens | 36 | 187.0 | 5.19 |
| Watercress | 21 | 120.0 | 5.71 |
| Napa (Chinese) cabbage | 13 | 77.0 | 5.92 |
| Turnip greens | 31.0 | 190.0 | 6.13 |
| Bok Choi (Chinese cabbage) | 11 | 68.8 | 6.26 |
|
Collard greens | 20 | 140.0 | 7.00 |
| Nopales (cactus leaves) | 22.0 | 164.0 | 7.46 |
| Lamb’s quarters | 34.0 | 309.0 | 9.09 |
| Mean | 28.9 | 67.6 | 2.56 |
Common Fruits and Their Mg and Ca Content
TABLE 2: calcium and magnesium content and calcium-to-magnesium ratio of common fruits sorted by ratio
|
Fruit | Mg/100g |
Ca/100g | Ca/Mg |
|---|---|---|---|
| Plantain | 37 | 3 | 0.08 |
| Banana | 27.0 | 5 | 0.19 |
| Star fruit | 10 | 3 | 0.30 |
| Passion fruit | 29 | 12 | 0.41 |
| Avocado | 29 | 12 | 0.41 |
| Lychees | 10 | 5 | 0.5 |
| Cherimoya | 17 | 10 | 0.59 |
| Honeydew melon | 10 | 6 | 0.60 |
| Cactus figs | 85 | 56 | 0.66 |
| Peach | 9 | 6 | 0.67 |
| Nectarine | 9 | 6.3 | 0.67 |
| Breadfruit | 25 | 17 | 0.68 |
| Watermelon | 10 | 7 | 0.70 |
| Cantaloupe | 12.0 | 9 | 0.75 |
| Guave | 22 | 18 | 0.82 |
| Pomegranate | 12 | 10 | 0.83 |
| Plum | 7 | 6 | 0.86 |
| Salmon berries | 15 | 13.1 | 0.87 |
| Persimmons | 9 | 8 | 0.89 |
| Payaya | 21.0 | 20 | 0.95 |
| Casaba melon | 11.0 | 11.0 | 1.00 |
| Blueberries | 6 | 6 | 1 |
| Pineapple | 12.0 | 13 | 1.08 |
| Mango | 10 | 11 | 1.1 |
| Raspberries | 22.0 | 25 | 1.14 |
| Oheloberries | 6 | 7 | 1.17 |
| Sweet cherry | 11 | 13.0 | 1.18 |
| Apple | 5 | 6 | 1.2 |
| Strawberries | 13.0 | 16 | 1.23 |
| Loganberries | 21 | 26 | 1.24 |
| Pear | 7 | 9 | 1.29 |
| Cranberries | 6 | 8 | 1.33 |
| Quince | 8 | 11 | 1.38 |
| Chayote | 12 | 17 | 1.41 |
| Grapes (Red or Green) | 7 | 10 | 1.43 |
| Blackberries | 20.0 | 29 | 1.45 |
| Boysenberries | 16 | 27 | 1.69 |
| Kiwi fruit | 17.0 | 34 | 2.00 |
| Mulberries | 18 | 39 | 2.17 |
| Chokecherries | 27 | 60 | 2.22 |
| Grapefruit | 9.0 | 22.0 | 2.44 |
| Gooseberries | 10 | 25 | 2.50 |
| Tangerine | 12.0 | 37.0 | 3.08 |
| Kumquats | 20 | 62 | 3.10 |
| Orange | 10 | 40 |
4.00 |
| Lemon | 12 | 61 | 5.08 |
| Lime | 6 | 33.0 | 5.50 |
| Elderberries | 5 | 38 | 7.6 |
| Mean | 10.6 | 14.0 | 1.5 |
Remember that it’s not the ratio of any one particular food, but the overall ratio of your daily diet that’s important. That said, making sure you eat foods with a low ratio to balance foods with a high ratio will help keep you in a healthy range.
And the best way to do that is to simply follow the guidelines in this article on 3 Micronutrient Ratios to Keep in Balance as well as visiting our great collection of recipes.
References
1. Carafoli E. Calcium signaling: A tale for all seasons. Proc National Acad Sci. 2002;99(3):1115–22.
2. Bilezikian JP, Bailey L, Elmer PJ, Favus MJ, Go VLW, Goldring SR, et al. Optimal Calcium Intake. Jama. 1994;272(24):1942–8.
3. Rosanoff A, Dai Q, Shapses SA. Essential Nutrient Interactions: Does Low or Suboptimal Magnesium Status Interact with Vitamin D and/or Calcium Status? Adv Nutrition Int Rev J. 2016;7(1):25–43.
4. Steck SE, Omofuma OO, Su LJ, Maise AA, Woloszynska-Read A, Johnson CS, et al. Calcium, magnesium, and whole-milk intakes and high-aggressive prostate cancer in the North Carolina–Louisiana Prostate Cancer Project (PCaP). Am J Clin Nutrition. 2018;107(5):799–807.
5. Cordain L. Dairy: Milking it for all it’s worth [Internet]. The Paleo Diet. 2014 [cited 2018 Nov 15]. Available from: https://thepaleodiet.com/dairy…;
6. Michaëlsson K, Melhus H, Lemming EW, Wolk A, Byberg L. Long term calcium intake and rates of all cause and cardiovascular mortality: community based prospective longitudinal cohort study. Bmj Br Medical J. 2013;346(feb12 4):f228.
7. Reid IR, Bolland MJ, Grey A. Does calcium supplementation increase cardiovascular risk? Clin Endocrinol. 2010;73(6):689–95.
8. Bolland MJ, Avenell A, Baron JA, Grey A, MacLennan GS, Gamble GD, et al. Effect of calcium supplements on risk of myocardial infarction and cardiovascular events: meta-analysis. Bmj. 2010;341(jul29 1):c3691.
9. MALCOLM DS, ZALOGA GP, HOLADAV JW. Calcium administration increases the mortality of endotoxic shock in rats. Crit Care Med. 1989;17(9):900–3.
10. Sahmoun AE, Singh BB. Does a higher ratio of serum calcium to magnesium increase the risk for postmenopausal breast cancer? Med Hypotheses. 2010;75(3):315–8.
11. Xiao Q, Murphy RA, Houston DK, Harris TB, Chow W-H, Park Y. Dietary and Supplemental Calcium Intake and Cardiovascular Disease Mortality: The National Institutes of Health–AARP Diet and Health Study. Jama Intern Med. 2013;173(8):639–46.
12. Green JH, Booth C, Bunning R. Impact of supplementary high calcium milk with additional magnesium on parathyroid hormone and biochemical markers of bone turnover in postmenopausal women. Asia Pac J Clin Nutr. 2002;11(4):268–73.
13. Kelly O, Gilman J, Ilich J. Utilizing Dietary Micronutrient Ratios in Nutritional Research May be More Informative than Focusing on Single Nutrients. Nutrients. 2018;10(1):107.
14. L. C. The nutritional characteristics of a contemporary diet based upon Paleolithic food groups. Journal of the American Nutraceutical Association. 2002;5:15–24.
15. Gobbo LCD, Imamura F, Wu JH, Otto MC de O, Chiuve SE, Mozaffarian D. Circulating and dietary magnesium and risk of cardiovascular disease: a systematic review and meta-analysis of prospective studies. Am J Clin Nutrition. 2013;98(1):160–73.
16. Chiuve SE, Korngold EC, Januzzi JL, Gantzer ML, Albert CM. Plasma and dietary magnesium and risk of sudden cardiac death in women. Am J Clin Nutrition. 2011;93(2):253–60.
17. Zhang W, Iso H, Ohira T, Date C, Tamakoshi A, Group JS. Associations of dietary magnesium intake with mortality from cardiovascular disease: The JACC study. Atherosclerosis. 2012;221(2):587–95.
18. Lewis JR, Calver J, Zhu K, Flicker L, Prince RL. Calcium supplementation and the risks of atherosclerotic vascular disease in older women: Results of a 5‐year RCT and a 4.5‐year follow‐up. J Bone Miner Res. 2011;26(1):35–41.
19. Artaud-Wild SM, Connor SL, Sexton G, Connor WE. Differences in coronary mortality can be explained by differences in cholesterol and saturated fat intakes in 40 countries but not in France and Finland. A paradox. Circulation. 2018;88(6):2771–9.
20. ALCOCK N, MACINTYRE I. Inter-relation of calcium and magnesium absorption. Clin Sci. 1962;22:185–93.
21. Nadler JL, Buchanan T, Natarajan R, Antonipillai I, Bergman R, Rude R. Magnesium deficiency produces insulin resistance and increased thromboxane synthesis. Hypertension. 2018;21(6_Pt_2):1024–9.
22. White R, Hartzell H. Effects of intracellular free magnesium on calcium current in isolated cardiac myocytes. Science. 1988;239(4841):778–80.
23. Zhang A, Cheng TPO, Altura BM. Magnesium regulates intracellular free ionized calcium concentration and cell geometry in vascular smooth muscle cells. Biochimica Et Biophysica Acta Bba – Mol Cell Res. 1992;1134(1):25–9.
24. D’Angelo EK, Singer HA, Rembold CM. Magnesium relaxes arterial smooth muscle by decreasing intracellular Ca2+ without changing intracellular Mg2+. J Clin Invest. 1992;89(6):1988–94.
25. SEELIG MS. The Requirement of Magnesium by the Normal Adult. Am J Clin Nutrition. 1964;14(6):342–90.
26. Bussière FI, Gueux E, Rock E, Mazur A, Rayssiguier Y. Protective effect of calcium deficiency on the inflammatory response in magnesium-deficient rats. Eur J Nutr. 2002;41(5):197–202.
27. Horner SM. Efficacy of intravenous magnesium in acute myocardial infarction in reducing arrhythmias and mortality. Meta-analysis of magnesium in acute myocardial infarction. Circulation. 2018;86(3):774–9.
28. Shah NC, Shah GJ, Li Z, Jiang X-C, Altura BT, Altura BM. Short-term magnesium deficiency downregulates telomerase, upregulates neutral sphingomyelinase and induces oxidative DNA damage in cardiovascular tissues: relevance to atherogenesis, cardiovascular diseases and aging. Int J Clin Exp Med. 2014;7(3):497–514.
29. Rasmussen HS, Aurup P, Goldstein K, McNair P, Mortensen PB, Larsen OG, et al. Influence of magnesium substitution therapy on blood lipid composition in patients with ischemic heart disease. A double-blind, placebo controlled study. Arch Intern Med. 1989;149(5):1050–3.
30. Young IS, McFarlane C, McEneny J. Oxidative modification of triacylglycerol-rich lipoproteins. Biochem Soc T. 2003;31(5):1062–5.
31. Sluijs I, Czernichow S, Beulens JWJ, Boer JMA, Schouw YT van der, Verschuren WMM, et al. Intakes of Potassium, Magnesium, and Calcium and Risk of Stroke. Stroke. 2014;45(4):1148–50.
32. Zidverc-Trajković J, Pavlović AM, Jovanović Z, Šternić N, Kostić VS. Efficacy of intravenous magnesium sulfate in severe migraine attacks. J Headache Pain. 2001;2(2):79–82.
33. Clarkson EM, Warren RL, McDonald SJ, Wardener HE de. The effect of a high intake of calcium on magnesium metabolism in normal subjects and patients with chronic renal failure. Clin Sci. 1967;32(1):11–8.
34. Sojka J, Wastney M, Abrams S, Lewis SF, Martin B, Weaver C, et al. Magnesium kinetics in adolescent girls determined using stable isotopes: effects of high and low calcium intake. Am J Physiology-regulatory Integr Comp Physiology. 1997;273(2):R710–5.
35. Wagner CL, Greer FR, Breastfeeding AA of PS on, Nutrition AA of PC on. Prevention of Rickets and Vitamin D Deficiency in Infants, Children, and Adolescents. Pediatrics. 2008;122(5):1142–52.
36. Dai Q, Zhu X, Manson JE, Song Y, Li X, Franke AA, et al. Magnesium status and supplementation influence vitamin D status and metabolism: results from a randomized trial. Am J Clin Nutrition. 2018;108(6):1249–58.
37. Seelig MS. Increased need for magnesium with the use of combined oestrogen and calcium for osteoporosis treatment. Magnesium Res. 1990;3(3):197–215.
38. Deng X, Song Y, Manson JE, Signorello LB, Zhang SM, Shrubsole MJ, et al. Magnesium, vitamin D status and mortality: results from US National Health and Nutrition Examination Survey (NHANES) 2001 to 2006 and NHANES III. Bmc Med. 2013;11(1):187.




