The Mechanisms of Migraine Headaches

If you’ve ever suffered from migraine headaches, then you understand the pain. In some cases, the pain can be so severe that it can feel like your head is literally imploding—or exploding. [1]
For some sufferers, migraines can be severe enough that they become acutely disabled. In other words, they cannot go to work or enjoy their favorite activity because they must lay down in a dark, quiet room to confront the pain.
A surprising 18 percent of women and 6 percent of men in America suffer from migraine headaches. [1] Most doctors will likely give you a prescription for migraines; there’s a good chance diet will not be discussed at all. In this article, we explore ways that diet and supplements can cause (or help mitigate) migraine headaches.
Diet has the ability to both reduce inflammation and improve mitochondria function, which can eliminate migraine expression for many sufferers.
The Mechanism of Migraines
In 1999, I wrote a detailed article on the scientific mechanisms of pain. [2] It was cited in 2001 by the Director of the Pain Management Center at Brigham and Women’s Hospital, [3] which is one of Harvard Medical School’s teaching hospitals. What follows is a simplified explanation of pain and how it manifests, which is important to understand in order to manage migraines.
Humans and other animals have a central and peripheral nervous system. The central nervous system contains the spinal cord, brainstem, and brain. The brainstem is about three inches long and is located between the spinal cord and brain.
Nerve cells are called neurons. The peripheral nervous system contains two types of neurons, ones that transmit information from the central nervous system to the periphery, which are called motor neurons. As the name implies, motor neurons are involved in movement. If you are sitting in a chair and decide to get up, your motor neurons activate your muscles so you can move.
In contrast with motor neurons, sensory neurons respond to sensory stimuli such as touch and smell, and transmit that information from the periphery to the central nervous system and, ultimately, to specific regions in the brain. Our sensory neurons are so specialized that we can feel the lightest of touch, such as a tiny little bug crawling on an arm or leg.
We also have specialized neurons, called nociceptors, that respond only to noxious (unpleasant) stimuli. Nociceptors are found throughout the body, which is why almost all tissues in the body can become painful.
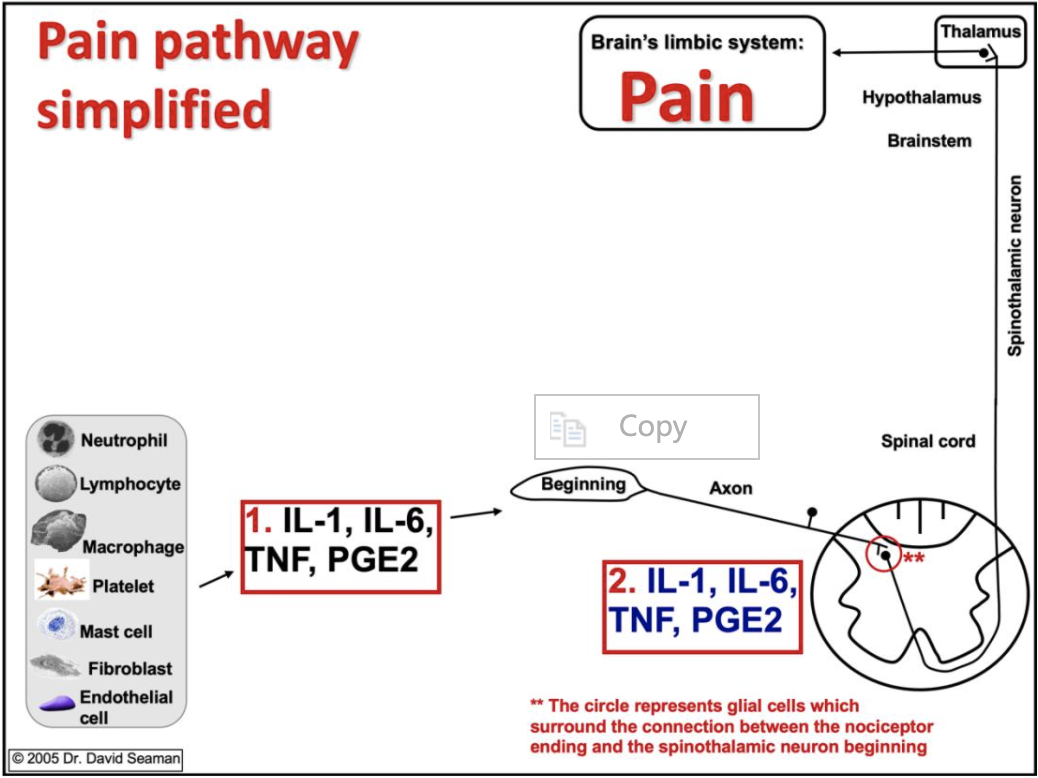
Figure 1 illustrates a nociceptor, which has a beginning, an axon, and an ending in the spinal cord. When a tissue experiences a noxious stimulus, cells such as neutrophils and endothelial cells release inflammatory chemicals that activate the nociceptor (including inflammatory cytokines such as IL-1 (interleukin-1), IL-6 (interleukin-6), and TNF (tumor necrosis factor.)
One chemical of particular note is PGE2 (prostaglandin E2) because it is directly influenced by our diets. (More on this later.) These chemicals activate nociceptors in joints, muscles, discs, tendons, bone, and certain visceral organs that become painful.
There is one major distinction between head pain and pain elsewhere in the body. While most pain is transmitted from nociceptors to the central nervous system through spinothalamic neurons, the neurons involved in head pain are called trigeminothalamic neurons.
The major distinguishing factor for migraine headache pain, versus most all other pains in the body, including run-of-the-mill headaches, is the fact that migraineurs have a genetic hyperexcitability in an area of the brainstem called the migraine generator, which increases the excitability of these trigeminothalamic neurons. [4]
Most people with migraine headaches will tell you that certain sensory stimuli will help to induce their migraines, such as certain foods, atmospheric changes, and/or exposure to particular odors, sounds, and light. These stimuli serve to activate the already overexcitable trigeminothalamic neurons and lead to a migraine attack. This means that migraineurs should identify and avoid their specific triggers.
Factors to Reduce the Prevalence of Migraines
It’s important for migraineurs to understand that their central nervous system is essentially wired to create migraine headaches. In other words, it is hyperexcitable and easily responds to triggers. To avoid pain, it needs to be kept calm.
Family history plays a big part in why this is. About 70 percent of people with migraines have family members who also suffer. Indeed, family history is the most potent and consistent risk factor of migraines. [5] Before you feel genetically doomed, however, keep in mind that there are two key factors you can control to help keep your nervous system “calm”:
- Reduce chronic inflammation
- Improve cell energy production
Let’s start with ways to reduce inflammation. As discussed earlier in this article, nociceptor neurons are stimulated by inflammation—or, more specifically, inflammatory cytokines such as IL-1 and IL-6. This means that migraineurs need to judiciously reduce their inflammatory state. Four key lifestyle factors influence inflammation:
- Chronic stress
- Lack of adequate sleep
- Physical inactivity
- The standard modern diet
These factors all work together to increase chronic inflammation, which increases the excitability of peripheral and central nociceptor neurons. The end result is the expression of many forms of pain, including migraine headaches.
When it comes to energy, the vast majority of cellular energy is produced by specialized structures called mitochondria. Migraineurs appear to have compromised mitochondria, which leads to less energy production. In essence, the nervous system perceives this as a cellular energy crisis that leads to an increase in the excitability of the hypothalamus-brainstem-trigeminothalamic region that drives migraine expression. [6]
Diet has the ability to both reduce inflammation and improve mitochondria function, which can eliminate migraine expression for many sufferers. With this in mind, it is important to understand that some people only need to make minor improvements to get relief, while others have to pursue a more fully “DeFlamed” state, as I refer to it. For these sufferers, major lifestyle improvements must be maintained to get relief.
The standard American diet is a migraine-promoting diet. And when people live on this pro-inflammatory diet for protracted periods of time, several pro-inflammatory biological changes can occur in the body that serve to literally anchor migraine headaches as a permanent condition.
In addition to inducing inflammation, the overconsumption of refined carbohydrates will suppress mitochondrial activity. In one study, healthy subjects aged 19-33 years were given approximately 140 grams of glucose per day for 4 weeks—the equivalent of about 40 ounces of cola soda per day. This led to a reduction in mitochondrial energy production [11], which is exactly what migraineurs do not want.
Readers familiar with The Paleo Diet should also know that a key goal is to avoid foods with an excess of omega-6 fatty acids. It turns out that this, too, is very important for preventing migraine headaches. Refined seed oils (corn, safflower, sunflower, cottonseed) and legume oils (peanut and soybean) contain an abundance of omega-6 linoleic acid and are used in deep fryers and in most packaged food products.
Shockingly, the average American gets almost 20 percent of their total calories from these omega-6 oils, which results in an omega-6 to omega-3 ratio of at least 10:1, which is pro-inflammatory. [12] The proper ratio to achieve an anti-inflammatory state is less than 4:1.
When we consume omega-6 linoleic acid, our bodies convert it into omega-6 arachidonic acid and store it in cell membranes. This is highly problematic for migraineurs as arachidonic is converted into a pro-inflammatory chemical known as prostaglandin E2 (PGE2).
For perspective, the main reason people take aspirin and other similar non-steroidal anti-inflammatory drugs (NSAIDs) is because these drugs inhibit pain by stopping the conversion of arachidonic acid into PGE2. With this in mind, consider the following conclusion from a study published in 2012:
“We suggest that PGE2 may be one of the important final products involved in the generation of migraine attacks.” [13]
To put this into perspective, the average American gets almost 60 percent of their calories from refined sugar, flour, and oils, which increase inflammation in general and PGE2 specifically, in addition to depressing mitochondrial activity.
This means that the standard American diet is a migraine-promoting diet. And when people live on this pro-inflammatory diet for protracted periods of time, several pro-inflammatory biological changes can occur in the body that serve to literally anchor migraine headaches as a permanent condition. These changes include obesity, gut dysbiosis, and activation of the kynurenine pathway.
Obesity creates a chronic pro-inflammatory state, which promotes most chronic diseases, including migraine headaches. A recent study found that obese individuals were three times more likely to suffer with migraine headaches compared to normal weight individuals. [14]
Changes in the gut flora occur when we eat a pro-inflammatory diet. Gram-negative bacteria release an endotoxin called lipopolysaccharide, which can be absorbed into circulation and stimulate inflammation. [15,16] People with irritable bowel syndrome suffer from a state of low-grade endotoxemia and so are more likely to have migraine headaches. [17]
People with Celiac disease are also more likely to have migraine headaches, which means that trying a gluten-free diet is advisable [17], which one naturally does if The Paleo Diet is strictly adhered to.
Inflammation can also affect the kynurenine pathway. Normally, the amino acid tryptophan is converted into serotonin and then melatonin, which is why it is often supplemented by people with depression or sleep problems. Tryptophan can also be used by the kynurenine pathway where it is converted into the B-vitamin niacin.
Normally these pathways work in unison, but in a diet-induced inflammatory state, the kynurenine pathway can be overstimulated. This will cause it to steal tryptophan from the serotonin and melatonin pathways and overproduce pro-inflammatory anthranilic acid. It turns out that migraine patients have measurably elevated levels of pro-inflammatory anthranilic acid in circulation. [18]
Supplements That Might Reduce Migraines
We generally do not promote supplements. However, for some migraineurs, the pain is significant enough to need additional help, and supplements can have far less severe side effects compared to medication such as regular NSAID use. Further, while not many conditions can be substantially improved by taking nutritional supplements, in the case of migraine headaches, many people are able to significantly reduce their headaches.
Not surprisingly, these supplements reduce inflammation and support mitochondrial function. Fortunately, most of these supplements are relatively inexpensive.
A recent comprehensive review of migraine research [20] suggests that migraine headache patients should supplement with omega-3 fatty acids, probiotics, and vitamin D. All three supplements have anti-inflammatory benefits.
As most nutritionally minded people know, dietary omega-3 fatty acids in utero can help support proper brain development in early life. Omega-3 fatty acids also increase the proliferation of key gut probiotic bacteria, namely Lactobacillus and Bifidobacterium. [20] These bacteria can be lost during diet-induced dysbiosis leading to endotoxemia and chronic inflammation, two key drivers of migraine expression.
When migraineurs were supplemented with either a multispecies probiotic or placebo for 10 weeks, there was a significant reduction in migraine days for only the probiotic supplemented group. [22] The number of attacks per month was cut in half in the supplemented group while there was no improvement in the placebo group.
The omega-3 to omega-6 is a critical ratio in our diets and increasing omega-3 intake while reducing omega-6 intake can help prevent migraine headaches more than merely reducing one’s dietary intake of omega-6 fatty acids alone. [20] The typical supplemental dose of omega-3 fatty acids is 1-3 grams of eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). [21]
Vitamin D is not actually a vitamin; rather, it is a hormone that researchers characterize as “a pluripotent, pleiotropic seco-steroid with as many mechanisms of action as the 1,000 human genes it regulates.” [23]
In short, vitamin D regulates a host of pro-inflammatory and anti-inflammatory functions, so it is not surprising that migraine patients who are vitamin D deficient have more frequent attacks. [24] Supplementation of vitamin D3 should be based on an individual’s vitamin D level as measured by 25(OH)D. The normal range is 32-100 ng/ml. Many vitamin D researchers suggest that we all achieve levels of at least 40 ng/ml. My personal feeling is that we should go higher and achieve at least 60 ng/ml, and as long as serum calcium levels remain normal, we can achieve higher levels. This typically requires people to take from 2000-10,000 IUs of vitamin D3 per day.
Omega-3 fatty acids from fish oil, probiotics, and vitamin D clearly have anti-inflammatory and anti-endotoxin effects. In contrast, while magnesium and coenzyme Q10 (CoQ10) do have anti-inflammatory effects, they also promote mitochondrial function and reduce the frequency of migraine headaches. [25]
Several studies have evaluated the effectiveness of supplemental magnesium in migraineurs at doses of 500-600 mg/d, which was shown to reduce the severity and frequency of attacks. [25] In addition to supporting mitochondrial function, magnesium also is the key mineral that modulates the activity of NMDA receptors in the central nervous system. These receptors play a key role in nociceptive transmission and pain generation. A lack of magnesium increases the excitability of the NMDA receptors. [25]
Many people can tolerate more than 600 mg/d and so should be encouraged to find the dose that helps to best reduce migraine attack severity and frequency. Too much magnesium will most commonly cause diarrhea and/or abdominal pain and nausea.
CoQ10 is a key coenzyme involved in mitochondrial function. Several studies have evaluated the effectiveness of CoQ10 for reducing the severity and frequency of attacks and found the optimal dose to be between 100-400 mg per day. [25]
Some people may derive a greater benefit if higher doses are taken. In this context, a non-migraine-specific risk assessment for CoQ10 supplementation identified that intakes as high as 1,200 mg per day are safe. [26] We recommend starting in the 100-400 mg per day range.
Magnesium and CoQ10 are my preferred supplements for supporting mitochondrial function as they have diverse physiological benefits beyond a relationship to migraine headaches.
Magnesium is involved with over 300 metabolic reactions and its deficiency is associated with diverse clinical effects, such as inefficient memory, depression, cardiovascular disease, hypertension, stroke, osteoporosis, diabetes mellitus, asthma, and even sudden death. [27-29] Regarding CoQ10, the following quote is from the chapter about nutritional supplements in my book The DeFlame Diet:
“For CoQ10, I take the common recommended amount, which is 100 mg per day. Supplemental coenzyme Q10 (CoQ10) has become very popular in recent years for the following reasons. CoQ10 functions primarily to produce ATP (adenosine triphosphate), reduce free radicals, and to regulate skeletal muscle gene expression. [30-32] Nearly every disease studied has been shown to be associated with a reduction in ATP and an increase in free radicals, which makes CoQ10 an ideal supplement. When the Mediterranean diet was supplemented with CoQ10, there was an additional measurable reduction of inflammation. [33,34]”
The Bottom Line
In summary, my view is that people with migraine headaches should DeFlame their diets, which is the physiological outcome of The Paleo Diet, and also explore supplemental fish oil, probiotics, vitamin D, magnesium, and CoQ10 to see if they assist in reducing, and hopefully help to eliminate, the expression of migraine headaches.
References
1. Files JA, Schwedt TJ, Mayer AP, et al. Imploding and exploding migraine headaches: comparison of methods used to diagnose pain directionality. Headache. 2014;54:1010-18.
2. Seaman DR, Cleveland C. Spinal pain syndromes: nociceptive, neuropathic, and psychologic mechanisms. J Manip Physiol Ther. 1999;22:458-72.
3. Ross E. Moving towards a rational pharmacological management of pain with an improved classification system of pain. Expert Opin Pharmacol. 2001;2:1529-30.
4. Schulte LH, May A. The migraine generator revisited: continuous scanning of the migraine cycle over 30 days and three spontaneous attacks. Brain. 2016;139(Pt 7):1987-93
5. Lateef TM, Cui L, Nakamura E, et al. Accuracy of family history reports of migraine in a community-based family study of migraine. Headache. 2015;55:407-12.
6. Fila M, Pawtowska E, Blasiak J. Mitochondria in migraine pathophysiology – does epigenetics play a role? Arch Med Sci. 2019;15:944-56.
7. Dickinson S, Hancock DP, Petocz P, Ceriello A, Brand-Miller J. High–glycemic index carbohydrate increases nuclear factor- κB activation in mononuclear cells of young, lean healthy subjects. Am J Clin Nutr. 2008;87(5):1188-93.
8. Amar J, Burcelin R, Ruidavets JB, et al. Energy intake is associated with endotoxemia in apparently healthy men. Am J Clin Nutr. 2008;87(5):1219-23.
9. O’Keefe JH, Gheewala NM, O’Keefe JO. Dietary strategies for improving post-prandial glucose, lipids, inflammation, and cardiovascular health. J Am Coll Cardiol. 2008;51(3):249-255.
10. O’Keefe JH, Bell DS. Postprandial hyperglycemia/hyperlipidemia (postprandial dysmetabolism) is a cardiovascular risk factor. Am J Cardiol. 2007;100:899-904.
11. Sartor F, Jackson MJ, Squillace C, et al. Adaptive metabolic response to 4 weeks of sugar-sweetened beverage consumption in healthy, lightly active individuals and chronic high glucose availability in primary human myotubes. Eur J Nutr. 2013;52(3):937-48.
12. Cordain L, Eaton SB, Sebastian A, et al. Origins and evolution of the Western diet: health implications for the 21st century. Am J Clin Nutr. 2005;81(2):341–354.
13. Antonova M, Wienecke T, Olesen J, Ashina M. Prostaglandin E2 induces immediate migraine-like attack in migraine patients without aura. Cephalgia. 2012;32:822-33.
14. Miri A, Nasiri M, Zonoori S, et al. The association between obesity and migraine in a population of Iranian adults: a case-control study. Diabetes Metabolic Syn. 2018;12:733-36.
15. Amar J, Burcelin R, Ruidavets JB, et al. Energy intake is associated with endotoxemia in apparently healthy men. Am J Clin Nutr. 2008;87(5):1219-23.
16. Kelly CJ, Colgan SP, Frank DN. Of microbes and meals: the health consequences of dietary endotoxemia. Nutr Clin Pract. 2012;27(2):215-25.
17. van Hemert S, Breedveld AC, Rovers JM, et al. Migraine associated with gastrointestinal disorders: review of the literature and clinical implications. Front Neurol. 2014;5:241.
18. Curto M, Lionetto L, Negro A, et al. Altered kyurenine pathway metabolites in serum of chronic migraine patients. J Headache Pain. 2016;17:47.
19. Seaman DR. The DeFlame Diet: DeFlame your Diet, Body, and Mind. Wilm, NC: Shadow Panther Press. 2016
20. Arzani M, Jahromi SR, Ghorbani Z, et al. Gut-brain axis and migraine headache: a comprehensive review. J Headache Pain. 2020;21:15.
21. Covington MB. Omega-3 fatty acids. Am Fam Phys. 2004;70:133-40.
22. Martami F, Togha M, Seifishahpar M, et al. The effects of a multispecies probiotic supplement on inflammatory markers and episodic and chronic migraine characteristics: a randomized double-blind controlled trial. Cephalgia. 2019;39:841-53.
23. Cannell JJ, Zasloff M, Garland CF, Scragg R, Giovannucci E. On the epidemiology of influenza. Virology J. 2008; 5:29.
24. Song TJ, Chu MK, Sohn JH, et al. Effect of vitamin D deficiency on the frequency of headaches in migraine. J Clin Neurol. 2018;14:366-73.
25. Nattagh-Eshtivani E, Sani MA, Dahri M, et al. The role of nutrients in the pathogenesis and treatment of migraine headaches: Review. Biomed Pharmacother. 2018;102:317-25.
26. Hathcock JN, Shao A. Risk assessment for coenzyme Q10 (ubiquinone). Reg Toxicol Pharmacol. 2006;45:282-88.
27. Wester PO, Dyckner T. The importance of the magnesium ion. Magnesium deficiency symptomatology and occurrence. Act Med Scand (suppl) 1982; 661:3-4.
28. Ford ES, Mokdad AH. Dietary magnesim intake in a national sample of US adults. J Nutr. 2003; 133:2879-82.
29. Bar-Dayan Y, Shoenfield Y. Magnesium fortification of water. A possible step forward in preventive medicine? Ann Med Interne (Paris). 1997;148(6):440-4.
30. Crane FL. Biochemical functions of coenzyme Q10. J Am Coll Nutr. 2001; 20:591-98.
31. Linnane AW, Zhang C, Yarovaya N et al. Human aging and global function of coenzyme Q10. Ann NY Acad Sci. 2002; 959:396-411.
32. Linnane AW, Kopsidas G, Zhang C et al. Cellular redox activity of coenzyme Q10: effect of CoQ10 supplementation on human skeletal muscle. Free Rad Res. 2002;36:445-453.
33. Yubero-Serrano EM, Delgado-Casado N, Delgado-Lista J et al. Postprandial antioxidant effect of the Mediterranean diet supplemented with coenzyme Q10 in elderly men and women. AGE. 2011;33:579-90.
34. Yubero-Serrano EM, Gonzalez-Guardia L, Rangel-Zungia O et al. Mediterranean diet supplemented with coenzyme Q10 modifies the expression of proinflammatory and endoplasmic reticulum stress—related genes in elderly men and women. J Gerontol A Biol Sci Med Sci. 2012;67A(1):3–10




