Evolution and High Protein Diets Part 3

Did you miss Evolution and High Protein Diets Part 1? Click Here to Read It!
Did you miss Evolution and High Protein Diets Part 2? Click Here to Read It!
Dietary protein: health and well-being
Establishing Cause and Effect between Diet and Disease
One of the challenges faced by nutritional scientists when they ultimately make recommendations regarding what we should and should not eat is to establish cause and effect between a dietary element and the subsequent development or prevention of disease. Some foods and some dietary habits promote good health, whereas others promote disease.
No single procedure alone can establish cause and effect,65, 66 nor can any single study prove causality.67 Observational epidemiological studies can only show relationships among variables and are notorious for showing conflicting results68 and cannot provide decisive evidence by themselves either for or against specific hypotheses.69 For example, increased animal protein has been associated with a decreased risk for coronary heart disease (CHD) in a large group of nurses (The Nurses Health Study),70 whereas exactly the opposite association was found for markers of CHD and meat consumption in people from rural China.71, 72 An analogy here may be appropriate to show you why observational epidemiological studies can only show relationships and not establish causality. In New York City, there is a strong association between the size of a structure fire and the number of fire trucks at the fire, but can we conclude that more fire trucks cause bigger fires?
In order to establish cause and effect between diet and disease, it takes more than just observational epidemiological evidence.69 There must also be what is referred to as “biological plausibility” in which evidence gathered from tissue, animal and short term human metabolic studies support causality.66 When observational epidemiological evidence is augmented by biological plausibility studies and confirmed by randomized controlled trials, the case for causality becomes ever more convincing. In regard to optimal amounts of dietary protein, the bulk of the evidence from tissue and animal studies and from human dietary interventions provides a compelling case for the therapeutic effects of high protein diets.
Dietary Protein and Cardiovascular Disease
One of the reasons why observational epidemiological studies yield contradictory results is because of the influence of confounding variables, which cause confusion in the interpretation of the results because of the mixing of effects from two or more variables.68 For example, although some observational studies have shown a positive association between animal protein and cardiovascular disease (CVD), it is entirely possible that this association is spurious because the measurement of animal protein is confounded by another variable that is also linked to CVD. Meat is a major source of animal protein in the U.S. diet,20 but it is also a major source of saturated fat.73 Because meat comes as an inseparable package of (protein + saturated fat), animal protein ingestion will be highly correlated to saturated fat, thereby making it difficult to disengage the atherogenic effect of saturated fat from that of animal protein. Accordingly, experimental studies are more useful to determine the true effect that animal protein may have on cardiovascular risk factors because they can be designed to isolate the protein effects from the saturated fat effects.
Sinclair and colleagues74 performed an experiment in which they fed ten adults a low fat, lean beef-based diet for five weeks. Energy intake was kept constant over the five-week study. Total blood cholesterol concentrations fell significantly within one week of commencing the diet but rose as beef fat drippings were added in a stepwise manner in weeks four and five. The authors concluded, “. . . it is the beef fat, not lean beef itself, that is associated with elevations in cholesterol concentrations.”
Numerous short term human dietary interventions have demonstrated the therapeutic effect of lean, animal based protein upon blood lipid parameters. Wolfe and colleagues have shown that the isocaloric substitution of protein (23% energy) for carbohydrate in moderately hypercholesterolemic subjects resulted in significant decreases in total, LDL and VLDL cholesterol, and triglycerides while HDL cholesterol increased.75 Similar blood lipid changes have been observed in normal healthy subjects76 and in type II diabetic patients in conjunction with improvements in glucose and insulin metabolism.77, 78
A litany of more recent studies has confirmed that elevations in dietary protein have a beneficial effect upon blood lipid profiles.79-85 The mechanism or mechanisms of action of high protein diets upon blood lipid chemistry are not clear; however animal studies suggest that the beneficial effects are caused by their powerful inhibition of hepatic VLDL synthesis, perhaps by altering apoprotein synthesis and assembly in the liver.86
The relationship between protein intake and blood pressure has been comprehensively examined in observational population studies, and support the notion that higher protein intake can lower blood pressure.87-89 A substantial number of randomized controlled trials have demonstrated that higher dietary protein either from soy,90-92 mixed dietary sources85 or from lean red meat93 significantly lower blood pressure.
Dietary Protein and Insulin/Glucose Metabolism and Weight Regulation
In addition to reducing CVD risk by improving the blood lipid profile and reducing blood pressure, higher protein diets have been shown to improve insulin sensitivity and glycemic control79, 81, 84, 94-96 while promoting greater weight loss80, 83, 84, 97, 98 and improved long term sustained weight maintenance99, 100 than low fat high carbohydrate calorie restricted diets. The weight loss superiority of higher protein, calorie restricted diets over either calorie restricted (low fat/ high carbohydrate) diets or calorie restricted (high fat/low carbohydrate) appears to be caused by the greater satiety value of protein compared to either fat or carbohydrate.macronutrients (protein, fat, carbohydrate), protein causes the greatest release of a gut hormone (PYY) that reduces hunger103 while simultaneously improving central nervous system sensitivity to leptin,97 another hormone that controls appetite and body weight regulation.
Dietary Protein and Bone Health
One of the crucial issues regulating bone mineral health and integrity is calcium balance which represents the difference between the amount of dietary calcium which is absorbed and the amount of calcium leaving the body through the urine and feces. Figure 5 demonstrates two key points: 1) most (~75%) of dietary calcium is not absorbed, and 2) calcium absorption increases with decreasing dietary intakes and decreases with increasing dietary intakes.104
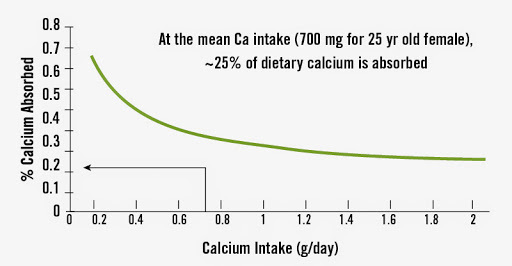
Figure 5. Relation between Calcium Intake and Absorption
Because dietary protein has been frequently, but not always,105-108 shown to increase urinary calcium excretion, it is possible that long term ingestion of high protein diets could lead to accelerated loss of calcium from the bones thereby impairing bone health and integrity.
Without the concurrent measurement of dietary calcium absorption along with urinary calcium losses the net calcium balance cannot be known. Hence, the simple observation that dietary protein ingestion may increase urinary calcium losses tells us little or nothing about calcium balance. In evaluating the effect of high protein diets upon bone mineral health, it is therefore crucial to measure both urinary calcium excretion and intestinal absorption of calcium. In this regard, Pannemans and colleagues109 compared a low protein (12% energy) to a high protein diet (21% energy) in young and elderly subjects. Both a higher urinary calcium excretion and a higher intestinal absorption of calcium were induced by the high protein diet, thus no negative calcium balance occurred.
A similar experiment confirmed that elevated dietary protein enhances calcium absorption and thereby counters the increased urinary excretion of calcium.110
Furthermore, a series of recent dietary interventions in humans has shown that high protein, meat based diets do not cause loss of calcium from the skeleton, but actually have a favorable effect upon it by lowering bone resorption105, 107, 111, 112 and may actually increase bone formation by dietary protein induced increases in IFG-1.105
Dietary Protein and Kidney Function
One of the most common misperceptions about high protein diets is that they can damage the kidneys of healthy normal individuals. This concept is known as the “Brenner Hypothesis”113 and suggests that increased dietary protein elevates the kidney’s filtration rate (GFR) which in turn alters the kidney’s structure (glomerulosclerosis) which then causes albumin to appear in the urine (microalbuminuria). Although these series of steps represent the hypothesis Brenner proffered,113 his experiments actually showed an entirely different series of events. In reality, Brenner demonstrated that patients with pre-existing kidney disease had an elevated GFR, glomerulosclerosis and microalbuminuria and that by reducing dietary protein the GFR and microalbuminuria could be lowered.113 He further suggested that because elevated dietary protein increased the GFR in short term studies (< 2 weeks) of healthy normal subjects, protein was responsible for kidney damage. The problem with this interpretation is that markers of functional kidney damage in the normal subjects (microalbuminuria) were not demonstrated along with the elevations in GFR, nor were any long term studies (3-6 months) carried out to determine if the kidneys adapted to a higher protein intake.
The incidence of diabetic end stage kidney disease has increased steadily over the past three decades.114, 115 If dietary protein were responsible for causing kidney damage, then one might expect that dietary protein would have steadily increased during this same time interval. In fact, dietary protein significantly increased in female subjects.118 The high protein diet did not cause urinary albumin to increase. Additionally, the specific GFR, which is an expression of the filtration rate per unit kidney volume, did not change during the high protein diet, indicating that renal (kidney) adaptation occurred to the higher protein load. The authors summarized, “We therefore conclude that a high dietary protein intake does not appear to have adverse effects on renal function in individuals without renal impairment.”
Dietary Protein and Cancer
Observational epidemiological studies frequently,119 but not always120 show that high animal protein diets may increase the risk for a variety of cancers, particularly colorectal cancer.121 Consequently, it might be expected that non-meat eating vegetarians would have a lower risk for these cancers. Paradoxically, this effect has not been consistently demonstrated.119 A proposed mechanism of action for the carcinogenic effect of meat consumption is the formation of toxic N-nitroso compounds (NOC) in the gut from heme iron in meat.122, 123 Short term human studies are in agreement that increased meat consumption increases NOC formation both in the lower122 and upper123 gastrointestinal tract. However, whether this situation translates into increased cancer risk is not known because to date, no randomized controlled trials of increased meat consumption in humans, using cancer diagnosis as an end point, have been conducted.
The meats and fish consumed by pre-agricultural humans were almost always fresh, whereas current western diets contain significant quantities of processed, salted meats and fish preserved with nitrites and nitrates. Processed meats contains 10 times more NOC (5.5 µmol/kg) than fresh meat (0.5 µmol/kg).124 Pre-agricultural humans consumed their fresh meats along with high intakes of fresh fruits and vegetables estimated to be between 35-45% of total energy14 compared to 8.1% of total energy in the current U.S. diet.125 Increased fruit and vegetable consumption decreases the fecal transit time so that NOC have less contact time with the colonic mucosa and therefore may reduce the carcinogenic risk.126 Hence, the context under which high meat consumption occurred in hunter-gatherers varied significantly from what occurs in westernized populations.
Animal based foods were almost always consumed fresh in conjunction with copious quantities of fresh fruits and vegetables. Even when vegetable intake was low or absent in these peoples, there is little evidence for an association of high protein, animal based diets with colorectal cancer. Prior to western acculturation, the Inuit may have consumed more than 95% of their daily energy from animal and seafood,15 yet a comprehensive review examining virtually all historical and ethnographic data of these people prior to westernization was unable to document a single case of colorectal cancer.126 Should a high protein meat based diet initiate or promote colorectal cancer, then one might expect obligate carnivores such as cats to demonstrate high incidences of these malignancies. In, fact the opposite is true, and the rate of gastrointestinal tract cancers is quite low in domestic cats.128 In summary the case for animal based, high protein diets causing colorectal cancer, within the context of pre-agricultural diets, is weak.
Dietary Protein and Muscle Protein Synthesis and Fatigue
For athletes and individuals engaging in regular exercise, an animal based, high protein diet may be ergogenic and facilitate improved performance because of the stimulatory effect of dietary branch chain amino acids (BCCA) upon muscle protein synthesis,129-131 particularly when they are consumed in the post exercise window.132, 133 Lean meats and fish are much richer sources of the branch chain amino acids (valine, leucine and isoleucine) than are plant foods. In addition to facilitating muscle synthesis during the post exercise recovery period, BCCA may also improve endurance performance by reducing perceived exertion and mental fatigue by reducing the synthesis of brain 5-hydroxytryptamine, a substance that may promote central fatigue.134
Dietary protein: Summary and conclusions
The evolutionary evidence indicates that so called “high protein diets” (20-30% total energy) and “very high protein diets” (30-40% total energy) actually represent the norm which conditioned the present day the human genome over more than 2 million years of evolutionary experience. The evolutionary template would predict that human health and well being will suffer when dietary intakes fall outside this range. Hence the current U.S. consumption of protein (15% total energy) may not optimally promote health and well being. There is now a large body of experimental evidence increasingly demonstrating that a higher intake of lean animal protein reduces the risk for cardiovascular disease, hypertension, dyslipidemia, obesity, insulin resistance, and osteoporosis while not impairing kidney function.




