Is Sea Salt Healthy?

Somehow, people in the Paleo community have been led to believe that added sea salt, table salt, or even Celtic salt can be safely included in contemporary Paleo diets with no long-term, adverse health effects, and that high salt intakes were a normal part of ancestral, hunter-gatherer diets. Is sea salt healthy? The science says that added salt is not healthy, even at moderate levels.
At least, this is a notion gaining popularity among many bloggers in the Paleosphere. But the internet is somewhat of a wild west of information that doesn’t go through the rigorous checks and balances of scientific publishing.
In contrast, scientists and physicians from the Paleo community, including S. Boyd Eaton (M.D.), Staffan Lindeberg (M.D., Ph.D.), Pedro Bastos (M.S., Ph.D. candidate) Lynda Frassetto (M.D.), Anthony Sebastian (M.D.), James O’Keefe (M.D.), myself (Ph.D.) and others, have largely rejected the notion that high salt intakes were typically present in ancestral hunter-gatherer diets. We believe that high consumption of sodium does indeed produce long-term, adverse health effects in contemporary people23-43. Re-evaluation from numerous avenues of previously published data indicates that high salt/sodium consumption by our hunter-gatherer ancestors would have been implausible, or rare at best.
Further, important new evidence from an extensive 20-year study of salt ingestion on mortality, supports the physiological argument that high dietary salt intakes produce adverse health effects53-55.
New Scientific Evidence: Salt Consumption Increases Adverse Health Risks at Even Moderate Levels.
In 2005, the U.S. Department of Health and Human Services recommended that adults in the U.S. consume no more than 2300 mg of sodium per day (5.8 grams of salt)44. Additionally, people in specific groups (those 51 years of age or older, people with high blood pressure, diabetes, kidney disease and adults of African American ethnicity should consume no more than 1500 mg of sodium per day (3.8 grams of salt)44. Other worldwide organizations including The American Heart Association45, the World Health Organization46 and the government of England and Wales46 have made similar recommendations to reduce dietary sodium.
Okay – scientific agencies and organizations worldwide have made near universal recommendations to reduce dietary sodium intake to 2300 mg per day, corresponding to 5.8 grams of salt. Admittedly, we have disagreed with these organizations on other recommendations – particularly dietary fat – however, 24-hour urinary tracking makes it much easier to study the effects of sodium consumption compared to nutrients like fat. So, in this case, we feel both the research and the Paleolithic template lines up well with the recommendations.
Yet, an article on one Paleo website stated, “I feel that the data supports an intake between 3000 and 7000 milligrams of sodium . . . per day”17. Other Paleo bloggers16 have made similar claims4-6, 7, 18, 19-22.
So, what are the health effects if you decide to eat salted foods and increase your sodium intake above 2300 mg/day as almost all of these bloggers4-6, 7, 18, 19-22 advise?
This is a question that even the scientific community has been exploring more extensively in recent years. Some researchers have suggested “U” or “J” shaped relationships may exist between sodium intake and cardiovascular disease (CVD) risk56-58, meaning that high sodium consumption increases the risk of CVD, but so does low sodium consumption. This “U” shaped relationship has led some scientists to suggest that we should consume more than the recommended daily allowance of sodium.
However, methodological issues exist with studies showing a “U” or “J” shaped relationship between CVD risk and sodium intake. First, these studies used overnight or spot urinary sodium evaluations rather than the “gold standard” 24-hour urinary sodium measurements. Hence considerable errors may exist in the estimation of dietary sodium intake in these studies56-58. This may invalidate their results53.
Second, these studies may have incorrectly attributed cause and effect. When a patient is diagnosed as hypertensive and at high risk for CVD, the primary recommendation of doctors practicing western medicine is to significantly reduce sodium intake. This recommendation could explain why low sodium intakes are associated with higher rates of CVD and the “U” or “J” shaped relationships exist. It appears that the low sodium consumption wasn’t causing CVD, but rather the disease was causing the low consumption53.
Most recently, a large randomized controlled trial (The TOPH trial) involving 3,126 subjects over a 24-year period, explored the health impact of sodium consumption while addressing the above two methodological issues with previous studies. The two TOPH randomized controlled trials – one for all-cause mortality53 and the other for cardiovascular disease (CVD) risk54 – employed the “gold standard” 24-hour urinary sodium collection procedure to estimate dietary sodium intake55. The researchers also did not include subjects who had been previously diagnosed as hypertensive55.
The results clearly showed an increased risk of all-cause mortality (death) with increasing sodium intake53. An important point stands out from this trial – the authors demonstrated that at even the lowest levels of sodium intake, a direct linear relationship existed with mortality (see Figure 1 below – click on it to expand).
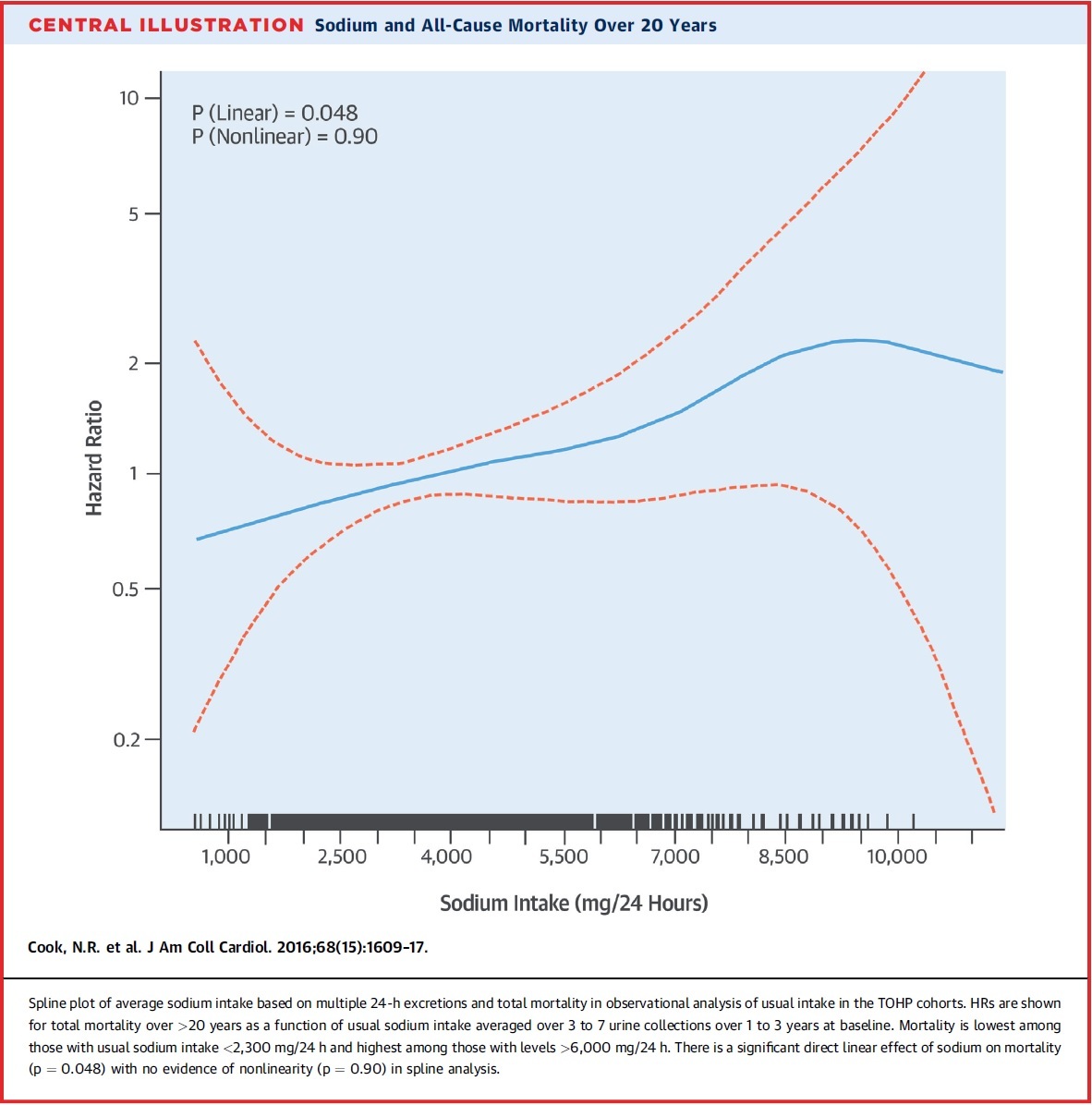
Figure 1: results of the TOPH study showing a linear relationship (blue line) between sodium consumption and all-cause mortality at all levels of sodium consumption53.
This information paints a grim picture about adding salt or sea salt to your diet. Your risk of dying from all causes increases proportionately with increased sodium intakes. The results of this study are consistent with an earlier TOPH trial, also demonstrating a linear and decreased risk of CVD, as sodium intake was lowered from 3600 mg/day to 2300 mg/d and then to 1500 mg/day54.
A recent meta-analysis (examination of multiple studies) of 34 randomized controlled trials of salt restriction, involving 3,230 participants and lasting for at least four weeks, showed a mean reduction in systolic blood pressure of 4.2 mm Hg with an accompanying decline in diastolic blood pressure of 2.1 mm Hg59. The authors concluded, “A modest reduction in salt intake for four or more weeks causes significant and, from a population viewpoint, important falls in blood pressure in both hypertensive and normotensive individuals, irrespective of sex and ethnic group”. Further, a meta-analysis of 13 prospective studies (following an event before it occurred and then after it occurred) involving 177,025 participants, demonstrated that a higher salt intake was associated with a greater risk of stroke60.
Further, many studies are revealing that the ratio of potassium to sodium in our diet is as important as sodium levels alone. A meta-analysis of eleven studies that included 247,510 male and female participants showed that higher daily potassium consumption was associated with a 21% reduction in the risk of stroke61.
Other Adverse Effects of High Salt Consumption
If you decide to not worry about sodium and cook with sea salt and refined salt, your risk of cardiovascular disease and all-cause mortality will increase. But these are not the only known adverse effects of adding mined sea salt and refined salt to your diet. Higher intakes of sodium increase the risk of certain cancers62-64, autoimmune and immune diseases65-68, as well as multiple diseases involving chronic low level, systemic inflammation65-70. Further high salt ingestion is known to disturb sleep patterns and cause insomnia71.
Sodium may also affect the length of our telomeres – the “caps” on the end of our DNA. Shortening of telomeres has been associated with aging72,73. A recent 2015 study found that salt consumption correlated with telomere length in overweight and obese adolescents. However, this study suffered from methodological issues tracking sodium consumption74.
Where’s the Salt?
Perhaps the best evidence for a low salt diet comes simply from inspection of the foods we eat. If high salt diets were a normal part of human physiology, then you would expect to find high concentrations of sodium in many of the natural, unsalted foods we eat. As we will shortly point out, nothing could be further from the truth. Almost all non-processed, non-salted foods in contemporary Paleo Diets contain low concentrations of sodium. Similarly, virtually, all wild, non-domesticated foods are quite low in sodium, as we will demonstrate in a future blog.
Fortunately, you don’t have to be a trained nutritionist to evaluate sodium in the USDA food tables and understand that high sodium foods are rarely or infrequently consumed in their natural, unsalted condition. This is simply because, with few exceptions, they don’t exist.
Let me summarize the USDA food data on sodium so you can see for yourself that it would be nearly impossible to consume a high salt diet on unadulterated natural foods. Table 1 below lists the sodium and potassium concentrations of contemporary foods in their natural, unsalted, unadulterated state:
Table 1. Sodium and potassium concentrations in contemporary natural foods.
(Click on table to see full size)
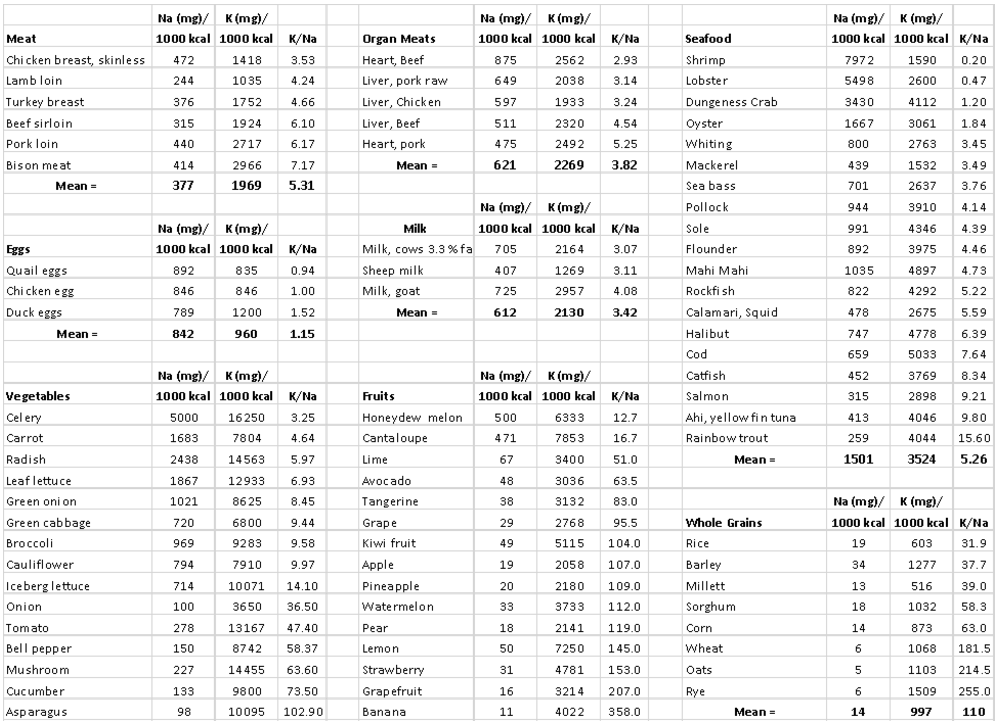
These food items are categorized by food groups (meat, organ meats, seafood, eggs, milk, vegetables, nuts and seeds, fruits, starchy roots, legumes, and whole grains). Note that three of these categories (whole grains, milk and legumes) are not included in contemporary Paleo diets. The various items in each of the 11 food categories were not selected randomly, but represent the most commonly consumed foods in the U.S. in each category. For instance, the 20 fruits listed in the “Fruits” category represent 20 of the most commonly consumed fruits in the U.S.
Important Points
A quick examination of Table 1 l shows that consumption of reasonable combinations of contemporary, unsalted, natural foods yields sodium intakes considerably lower than 2300 mg/day Note that suggested daily caloric intakes for women are 1600-2000 kcal/day and for men are 2400-2600 kcal/day.
Table 2 below averages the foods in each category from Table 1 to show daily sodium consumption for 11 food categories in men and women eating natural foods at normal daily caloric intakes without adding salt:
Table 2. Average sodium (Na) intakes for women eating between 1600 to 2000 kcal per day and for men eating between 2400 to 2600 kcal per day for 11 food categories if daily calories were met by eating only that food group.
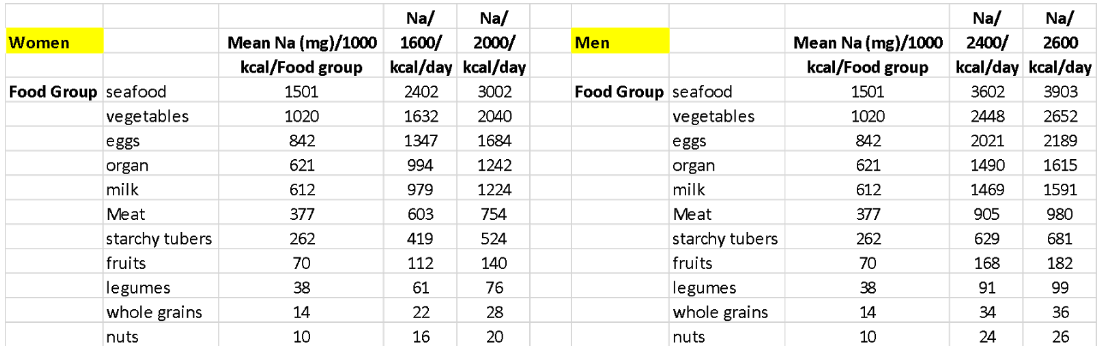
Table 2 shows that consumption of fresh, unprocessed foods, yields daily intakes of sodium which could have rarely or infrequently exceeded the governmental and institutional limits of 2300 mg/day. In fact, to exceed limits would require a diet consisting almost entirely of seafood and even then, the seafood would have to be primarily shellfish. It is also technically possible to slightly exceed recommendations eating only vegetables, but that would require eating a lot of celery. However, try eating enough celery in a day to hit 2300 mg of sodium – that’s 72 stalks! Perhaps 55 carrots sound more reasonable?
Are you starting to see the measures you’d have to go to on a natural diet with no added salt to exceed current sodium recommendations? Under normal food category selection by free-living people, sodium consumption would be significantly lower than the recommended daily allowance. So, readers I encourage you again to ask the simple question; “where’s the salt in natural unadulterated foods?”
Paleo dieters, consider this data. Fresh fruits contain a paltry 70 mg of sodium per 1000 calories on average, nuts supply only 10 mg of sodium per 1000 calories on average, fresh meat yields low concentrations of sodium (377 mg Na/1000 kcal), and fresh vegetables average only 1020 mg of sodium/1000 kcal.
Both Tables 1 and 2 show the implausibility of regularly consuming a combination of contemporary, normal foods on a regular basis, which would exceed 2300 mg of daily sodium. Reaching a sodium intake of 7000 mg/day, day after day, week after week, and month after month (as suggested by one Paleo blogger17, would be virtually impossible. These kinds of excessively high sodium intakes can only be achieved by adding mined sea salt, or processed salt47, 48 to natural, real foods. The Paleo Diet is not about adding salt, preservatives or any other additives to food, but rather about eating real, unprocessed foods as they occur naturally.
The Ratio of Potassium to Sodium: The Most Important Dietary Factor
Inclusion of a significant amount (35% to 45%) of plant food (fruits, vegetables, nuts, certain tubers – without added salt or sea salt) into your diet virtually assures a low sodium intake, no matter what else you eat. But more importantly from Table 1 you can see that if you eat natural, unsalted foods, potassium intakes will always greatly exceed sodium intakes under all normal food group selections.
High potassium consumption has been demonstrated to override the negative health effects of a high salt intake38, 49-52. Unfortunately, the typical western dietary pattern not only produces high sodium intakes, but also low potassium intakes, because we so infrequently eat high potassium foods such as fruits and vegetables. Worse, the western diet is high in sodium-enriched, potassium-depleted processed foods (particularly sugar, refined vegetable oils, margarines and processed fats) 26. So the message here is to reduce your sodium intake from processed food; don’t add salt or sea salt to your Paleo recipes, and definitely include more potassium rich plant foods (fruits, vegetables, nuts and seeds) into your diet.
The bottom line
Salt isn’t healthy and it isn’t Paleo, even if it’s sea salt.
There are a few key tips for keeping your body’s sodium levels in the healthy range:
- Limit your added salt intake. You can do this by severely reducing processed food. Only add sea salt to your Paleo recipes occasionally.
- Don’t worry about the natural sodium content of fresh meat or fish. They only contain moderate amounts of sodium.
- Include more potassium-rich plant foods into your diet. This includes fruits, vegetables, nuts, and seeds, and can help offset the amount of sodium you eat.
References
[1] Chatham John. Paleo for Beginners: Essentials to Get Started. Callisto Media (Publisher), Rockridge University Press (Imprint Publisher), Berkelely CA, 2012.
(Readers note: Rockridge University Press is an imprint publisher name assigned to this book, but it is actually produced by Callisto Media [//www.callistomedia.com/about.htm] which “utilizes proprietary algorithms to mine big data for topics of consumer interest and produces non-fiction titles”).
[2] No Author. Paleo Cookbook: 300 Delicious Paleo Diet Recipes. Callisto Media (Publisher), Rockridge University Press (Imprint Publisher), Berkelely CA, 2013.
(Readers note: Rockridge University Press Press is an imprint publisher name assigned to this book, but it is really produced by Callisto Media [//www.callistomedia.com/about.htm] which “utilizes proprietary algorithms to mine big data for topics of consumer interest and produces non-fiction titles”).
[3] Drummond M. The Paleo Slow Cooker Cookbook: 40 Easy to Prepare Paleo Recipes for Your Slow Cooker. CreateSpace Independent Publishing Platform, An Amazon Independent Publishing Company, 2014.
[4] Fragoso S. Everyday Paleo. Foreword by Robb Wolf. Victory Belt Publishing, Las Vegas NV, 2011.
[5] Gower C. Paleo Slow Cooking: Gluten Free Recipes Made Simple. Foreword by Robb Wolf. Victory Belt Publishing, Las Vegas NV, 2012.
[6] Mayfield J, Mayfield C. Paleo Comfort Foods: Homestyle Cooking for a Gluten-Free Kitchen. Foreword by Robb Wolf. Victory Belt Publishing, Las Vegas NV, 2011.
[7] Staley B, Mason H. Make it Paleo: Over 200 Grain-Free Recipes for Any Occasion. Foreword by Mark Sisson. Victory Belt Publishing, Las Vegas NV, 2011.
[8] //paleoleap.com/paleo-diet-recipes/
[9] //www.paleoplan.com/recipes/
[10] //paleogrubs.com/paleo-diet-recipes
[11] //blog.paleohacks.com/paleo-recipes/#
[12] //nomnompaleo.net/recipeindex/
[13] //www.paleonewbie.com/
[14] //paleoaholic.com/paleo-recipes/
[15] //paleomg.com/
[16] //thepaleodiet.com/charismatic-paleo-bloggers-rigorous-caution-required/
[17] Kresser C. Shaking Up The Salt Myth: Healthy Salt Recommendations. May 4, 2012. //chriskresser.com/shaking-up-the-salt-myth-healthy-salt-
recommendations/
[18] //www.marksdailyapple.com/salt-what-is-it-good-for/
[19] https://www.thepaleomom.com/is…
[20] //paleoleap.com/salt-and-a-paleo-diet/
[21] //www.paleoplan.com/ingredients/salt/
[22] //synergyhw.blogspot.com/2013/05/salt-one-of-your-best-friends-on-paleo.html
[23] Eaton SB, Konner M. Paleolithic nutrition. A consideration of its nature and current implications. N Engl J Med. 1985 Jan 31;312(5):283-9.
[24] Eaton SB, Konner M, Shostak M. Stone agers in the fast lane: chronic degenerative diseases in evolutionary perspective. Am J Med. 1988 Apr;84(4):739-49.
[25] Eaton SB, Eaton SB 3rd, Konner MJ. Paleolithic nutrition revisited: a twelve-year retrospective on its nature and implications. Eur J Clin Nutr. 1997 Apr;51(4):207-16.
[26] Cordain L, Eaton SB, Sebastian A, Mann N, Lindeberg S, Watkins BA, O’Keefe JH, Brand-Miller J. Origins and evolution of the Western diet: health implications for the 21st century. Am J Clin Nutr. 2005 Feb;81(2):341-54
[27] Konner M, Eaton SB. Paleolithic nutrition: twenty-five years later.
Nutr Clin Pract. 2010 Dec;25(6):594-602.
[28] Lindeberg S. Paleolithic diets as a model for prevention and treatment of Western disease. Am J Hum Biol. 2012 Mar-Apr;24(2):110-5.
[29] Jönsson T, Granfeldt Y, Ahrén B, Branell UC, Pålsson G, Hansson A, Söderström M, Lindeberg S. Beneficial effects of a Paleolithic diet on cardiovascular risk factors in type 2 diabetes: a randomized cross-over pilot study. Cardiovasc Diabetol. 2009 Jul 16;8:35 doi: 10.1186/1475-2840-8-35.
[30] Carrera-Bastos P, Fontes Villalba M, O’Keefe JH, Lindeberg S, Cordain L. The western diet and lifestyle and diseases of civilization. Res Rep Clin Cardiol 2011; 2: 215-235.
[31] Frassetto LA, Schloetter M, Mietus-Synder M, Morris RC, Sebastian A. Metabolic and physiologic improvements from consuming a paleolithic, hunter-gatherer type diet. Eur J Clin Nutr. 2015 Dec;69(12):1376. doi: 10.1038/ejcn.2015.193.
[32] Frassetto LA, Shi L, Schloetter M, Sebastian A, Remer T. Established dietary estimates of net acid production do not predict measured net acid excretion in patients with Type 2 diabetes on Paleolithic-Hunter-Gatherer-type diets. Eur J Clin Nutr. 2013 Sep;67(9):899-903
[33] Frassetto LA, Schloetter M, Mietus-Synder M, Morris RC Jr, Sebastian A. Metabolic and physiologic improvements from consuming a paleolithic, hunter-gatherer type diet. Eur J Clin Nutr. 2009 Aug;63(8):947-55.
[34] Frassetto LA, Morris RC Jr, Sellmeyer DE, Sebastian A. Adverse effects of sodium chloride on bone in the aging human population resulting from habitual consumption of typical American diets. J Nutr. 2008 Feb;138(2):419S-422S.
[35] Sebastian A, Frassetto LA, Sellmeyer DE, Morris RC Jr. The evolution-informed optimal dietary potassium intake of human beings greatly exceeds current and recommended intakes. Semin Nephrol. 2006 Nov;26(6):447-53.
[36] Frassetto L, Morris RC Jr, Sebastian A. Long-term persistence of the urine calcium-lowering effect of potassium bicarbonate in postmenopausal women. J Clin Endocrinol Metab. 2005 Feb;90(2):831-4.
[37] Sebastian A, Frassetto LA, Sellmeyer DE, Merriam RL, Morris RC Jr. Estimation of the net acid load of the diet of ancestral preagricultural Homo sapiens and their hominid ancestors. Am J Clin Nutr. 2002 Dec;76(6):1308-16.
[38] Frassetto L, Morris RC Jr, Sellmeyer DE, Todd K, Sebastian A. Diet, evolution and aging–the pathophysiologic effects of the post-agricultural inversion of the potassium-to-sodium and base-to-chloride ratios in the human diet. Eur J Nutr. 2001 Oct;40(5):200-13
[39] Morris RC Jr, Schmidlin O, Sebastian A, Tanaka M, Kurtz TW. Vasodysfunction That Involves Renal Vasodysfunction, Not Abnormally Increased Renal Retention of Sodium, Accounts for the Initiation of Salt-Induced Hypertension. Circulation. 2016 Mar 1;133(9):881-93
[40] Frassetto LA, Morris RC Jr, Sebastian A. Dietary sodium chloride intake independently predicts the degree of hyperchloremic metabolic acidosis in healthy humans consuming a net acid-producing diet. Am J Physiol Renal Physiol. 2007 Aug;293(2):F521-5.
[41] Morris RC Jr, Schmidlin O, Frassetto LA, Sebastian A. Relationship and interaction between sodium and potassium. J Am Coll Nutr. 2006 Jun;25(3 Suppl):262S-270S.
[42] Sellmeyer DE, Schloetter M, Sebastian A. Potassium citrate prevents increased urine calcium excretion and bone resorption induced by a high sodium chloride diet. J Clin Endocrinol Metab. 2002 May;87(5):2008-12.
[43] Sebastian A, Harris ST, Ottaway JH, Todd KM, Morris RC Jr. Improved mineral balance and skeletal metabolism in postmenopausal women treated with potassium bicarbonate. N Engl J Med. 1994 Jun 23;330(25):1776-81.
[44] Department of Agriculture, Department of Health and Human Services. Dietary guidelines for Americans, 2010. 7th ed. Washington, DC: Government Printing Office, December 2010.
[45] Whelton PK, Appel LJ, Sacco RL, et al. Sodium, blood pressure and cardiovascular disease: further evidence supporting the American Heart Association sodium reduction recommendations. Circulation 2012;126:2880-9.
[46] Cappuccio FP, Capewell S, Lincoln P, McPherson K. Policy options to reduce population salt intake. BMJ 2011;343: d4995.
[47] //thepaleodiet.com/sea-salt-devil-deep-blue-sea/
[48] //thepaleodiet.com/celtic-sea-salt/
[49] Morris RC Jr, Schmidlin O, Frassetto LA, Sebastian A. Relationship and interaction between sodium and potassium. J Am Coll Nutr. 2006 Jun;25(3 Suppl):262S-270S.
[50] Tobian L. Dietary sodium chloride and potassium have effects on the pathophysiology of hypertension in humans and animals. Am J Clin Nutr. 1997 Feb;65(2 Suppl):606S-611S.
[51] Manger WM, Simchon S, Stier CT Jr, Loscalzo J, Jan KM, Jan R, Haddy F. Protective effects of dietary potassium chloride on hemodynamics of Dahl salt-sensitive rats in response to chronic administration of sodium chloride. J Hypertens. 2003 Dec;21(12):2305-13.
[52] Cook NR, Obarzanek E, Cutler JA, Buring JE, Rexrode KM, Kumanyika SK, Appel LJ, Whelton PK; Trials of Hypertension Prevention Collaborative Research Group. Joint effects of sodium and potassium intake on subsequent cardiovascular disease: the Trials of Hypertension Prevention follow-up study. Arch Intern Med. 2009 Jan 12;169(1):32-40.
[53] Cook NR, Appel LJ, Whelton PK. Sodium Intake and All-Cause Mortality Over 20 Years in the Trials of Hypertension Prevention. J Am Coll Cardiol. 2016 Oct 11;68(15):1609-1617.
[54] Cook NR, Appel LJ, Whelton PK. Lower levels of sodium intake and reduced cardiovascular risk. Circulation. 2014 Mar 4;129(9):981-9.
[55] Ji C, Miller MA, Venezia A, Strazzullo P, Cappuccio FP. Comparisons of spot vs 24-h urine samples for estimating population salt intake: validation study in two independent samples of adults in Britain and Italy. Nutr Metab Cardiovasc Dis. 2014 Feb;24(2):140-7.
[56] O’Donnell M, Mente A, Rangarajan S, et al. Urinary sodium and potassium excretion, mortality, and cardiovascular events. N Engl J Med. 2014 Aug 14;371(7):612-23
[57] O’Donnell MJ, Yusuf S, Mente A, Gao P, Mann JF, Teo K, McQueen M, Sleight P, Sharma AM, Dans A, Probstfield J, Schmieder RE. Urinary sodium and potassium excretion and risk of cardiovascular events. JAMA. 2011 Nov 23;306(20):2229-38
[58] Pfister R, Michels G, Sharp SJ, Luben R, Wareham NJ, Khaw KT. Estimated urinary sodium excretion and risk of heart failure in men and women in the EPIC-Norfolk study. Eur J Heart Fail. 2014 Apr;16(4):394-402.
[59] He FJ1, Li J, Macgregor GA. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ. 2013 Apr 3;346:f1325. doi: 10.1136/bmj.f1325.
[60] Strazzullo P, D’Elia L, Kandala NB, Cappuccio FP. Salt intake, stroke, and cardiovascular disease: meta-analysis of prospective studies. BMJ. 2009 Nov 24;339:b4567. doi: 10.1136/bmj.b4567
[61] D’Elia L, Barba G, Cappuccio FP, Strazzullo P. Potassium intake, stroke, and cardiovascular disease a meta-analysis of prospective studies. J Am Coll
Cardiol. 2011 Mar 8;57(10):1210-9.
[62] D’Elia L, Rossi G, Ippolito R, Cappuccio FP, Strazzullo P. Habitual salt intake and risk of gastric cancer: a meta-analysis of prospective studies. Clin Nutr. 2012 Aug;31(4):489-98
[63] Ge S, Feng X, Shen L, Wei Z, Zhu Q, Sun J. Association between habitual dietary salt intake and risk of gastric cancer: A systematic review of observational studies. Gastroenterol Res Pract. 2012;2012:808120. doi: 10.1155/2012/808120. Epub 2012 Oct 22.
[64] Hu J, La Vecchia C, Morrison H, Negri E, Mery L; Canadian Cancer Registries Epidemiology Research Group. Salt, processed meat and the risk of cancer. Eur J Cancer Prev. 2011 Mar;20(2):132-9
[65] Kleinewietfeld M, Manzel A, Titze J, Kvakan H, Yosef N, Linker RA, Muller DN, Hafler DA. Sodium chloride drives autoimmune disease by the induction of pathogenic TH17 cells. Nature. 2013 Apr 25;496(7446):518-22
[66] Wu C, Yosef N, Thalhamer T, Zhu C, Xiao S, Kishi Y, Regev A, Kuchroo VK.
Induction of pathogenic TH17 cells by inducible salt-sensing kinase SGK1. Nature. 2013 Apr 25;496(7446):513-7.
[67] O’Shea JJ, Jones RG. Autoimmunity: Rubbing salt in the wound. Nature. 2013 Apr 25;496(7446):437-9.
[68] van der Meer JW1, Netea MG. A salty taste to autoimmunity. N Engl J Med. 2013 Jun 27;368(26):2520-1.
[69] Yi B, Titze J, Rykova M, Feuerecker M, Vassilieva G, Nichiporuk I, Schelling G, Morukov B, Choukèr A. Effects of dietary salt levels on monocytic cells and immune responses in healthy human subjects: a longitudinal study. Transl Res. 2015 Jul;166(1):103-10
[70] Zhou X1, Zhang L, Ji WJ, Yuan F, Guo ZZ, Pang B, Luo T, Liu X, Zhang WC, Jiang TM, Zhang Z, Li YM. Variation in dietary salt intake induces coordinated dynamics of monocyte subsets and monocyte-platelet aggregates in humans: implications in end organ inflammation. PLoS One. 2013 Apr 4;8(4):e60332. doi: 10.1371/journal.pone.0060332.
[71] Miller MM. Low sodium chloride intake in the treatment of insomnia and tension states. JAMA 1945;129: 262-266.
[72] Harley, C.B., A.B. Futcher, and C.W. Greider, TELOMERES SHORTEN DURING AGING OF HUMAN FIBROBLASTS. Nature, 1990. 345(6274): p. 458-460.
[73] Lopez-Otin, C., et al., The Hallmarks of Aging. Cell, 2013. 153(6): p. 1194-1217.
[74] Zhu, H., et al., High sodium intake is associated with short leukocyte telomere length in overweight and obese adolescents. International Journal of Obesity, 2015. 39(8): p. 1249-1253.